Tuesday Poster Session
Category: Small Intestine
P5021 - Duodenum in Distress: A Rare Case of Obstruction From Aortic Aneurysm
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio
- SB
Shoujit Banerjee, MD
University of California Irvine
Orange, CA
Presenting Author(s)
Shoujit Banerjee, MD1, Bryant Le, MD1, Andy L. Lin, MD2, Marie Balfour, MD2, Amirali Tavangar, MD2, Brian Mendoza, MD2, Peter H. Nguyen, MD2, Jason Samarasena, MD2, Frances Dang, MD2
1University of California Irvine, Orange, CA; 2University of California, Irvine, Orange, CA
Introduction: Aortoduodenal syndrome is an uncommon pathologic process due to duodenal obstruction from an enlarged aortic aneurysm. Patients may present with abdominal pain, weight loss, nausea, and vomiting. Although a rare diagnosis, it should be considered in patients with the appropriate risk factors such as history of abdominal aortic aneurysm (AAA), male sex, and age > 60.
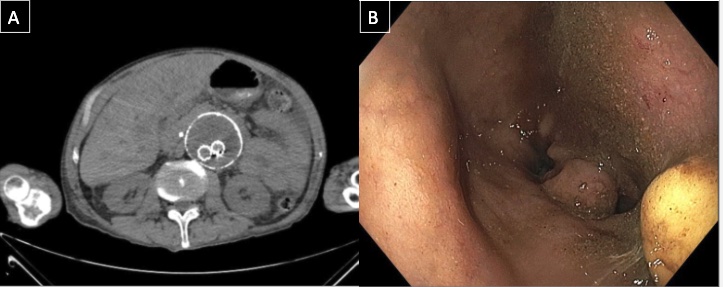
Case Description/Methods: A 66-year-old male with history of abdominal aneurysm status post EVAR, COPD, HTN, prior abdominal hernia repair presented to an outside hospital for abdominal pain and obstructive jaundice. He underwent EUS/ERCP, which found a malignant-appearing stricture and a biliary stent was placed. After discharge, he underwent EGD/EUS with FNA, but neither the scope nor wire could pass through the stricture to the duodenum, likely due to external obstruction. A 12x 9 mm liver lesion was biopsied during the procedure, revealing metastatic adenocarcinoma with GI or pancreatic origin. CT imaging post-procedure was concerning for a 6.6 cm AAA sac with mass effect on the pancreas, leading to compression of the gastric antrum and proximal duodenum (Figure A). CT-angiogram of the aorta did not reveal endovascular leak, with no vascular intervention. A repeat EGD/EUS was done to attempt gastrojejunostomy placement, but the scope could not traverse the duodenum (Figure B). The patient was planned for outpatient liver biopsy but re-admitted for failure to thrive. Given the poor prognosis of his cancer, he had extensive goals of care discussion and opted for home hospice. The patient passed away a few days after discharge.
Discussion: This case highlights the unique challenges in recognizing and managing aortoduodenal syndrome, particularly in the context of concurrent malignancy. Proposed mechanisms include direct compression of the duodenum or the super mesenteric artery (SMA) from the AAA. Although mass effect from the AAA was noted to be on the pancreas, downstream effects with compression of the proximal duodenum led to symptoms of gastric outlet obstruction. Clinicians should consider aortoduodenal syndrome in patients with a known history of AAA, a pulsatile abdominal mass, and vomiting. Treatment can range from gastric decompression and electrolyte correction to more definitive measures such as aortic graft placement.
Disclosures:
Shoujit Banerjee, MD1, Bryant Le, MD1, Andy L. Lin, MD2, Marie Balfour, MD2, Amirali Tavangar, MD2, Brian Mendoza, MD2, Peter H. Nguyen, MD2, Jason Samarasena, MD2, Frances Dang, MD2. P5021 - Duodenum in Distress: A Rare Case of Obstruction From Aortic Aneurysm, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of California Irvine, Orange, CA; 2University of California, Irvine, Orange, CA
Introduction: Aortoduodenal syndrome is an uncommon pathologic process due to duodenal obstruction from an enlarged aortic aneurysm. Patients may present with abdominal pain, weight loss, nausea, and vomiting. Although a rare diagnosis, it should be considered in patients with the appropriate risk factors such as history of abdominal aortic aneurysm (AAA), male sex, and age > 60.
Case Description/Methods: A 66-year-old male with history of abdominal aneurysm status post EVAR, COPD, HTN, prior abdominal hernia repair presented to an outside hospital for abdominal pain and obstructive jaundice. He underwent EUS/ERCP, which found a malignant-appearing stricture and a biliary stent was placed. After discharge, he underwent EGD/EUS with FNA, but neither the scope nor wire could pass through the stricture to the duodenum, likely due to external obstruction. A 12x 9 mm liver lesion was biopsied during the procedure, revealing metastatic adenocarcinoma with GI or pancreatic origin. CT imaging post-procedure was concerning for a 6.6 cm AAA sac with mass effect on the pancreas, leading to compression of the gastric antrum and proximal duodenum (Figure A). CT-angiogram of the aorta did not reveal endovascular leak, with no vascular intervention. A repeat EGD/EUS was done to attempt gastrojejunostomy placement, but the scope could not traverse the duodenum (Figure B). The patient was planned for outpatient liver biopsy but re-admitted for failure to thrive. Given the poor prognosis of his cancer, he had extensive goals of care discussion and opted for home hospice. The patient passed away a few days after discharge.
Discussion: This case highlights the unique challenges in recognizing and managing aortoduodenal syndrome, particularly in the context of concurrent malignancy. Proposed mechanisms include direct compression of the duodenum or the super mesenteric artery (SMA) from the AAA. Although mass effect from the AAA was noted to be on the pancreas, downstream effects with compression of the proximal duodenum led to symptoms of gastric outlet obstruction. Clinicians should consider aortoduodenal syndrome in patients with a known history of AAA, a pulsatile abdominal mass, and vomiting. Treatment can range from gastric decompression and electrolyte correction to more definitive measures such as aortic graft placement.
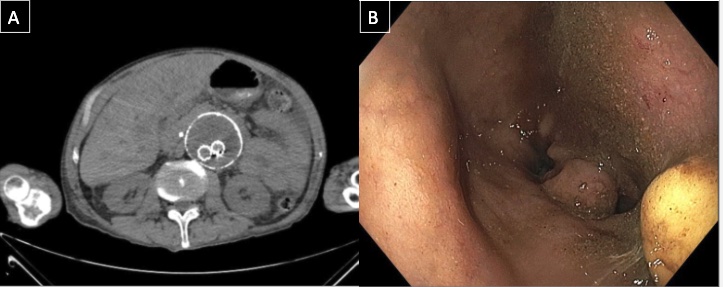
Figure: A. CT imaging demonstrating enlarging aortic aneurysm.
B. Endoscopic view of external duodenal obstruction.
B. Endoscopic view of external duodenal obstruction.
Disclosures:
Shoujit Banerjee indicated no relevant financial relationships.
Bryant Le indicated no relevant financial relationships.
Andy Lin indicated no relevant financial relationships.
Marie Balfour indicated no relevant financial relationships.
Amirali Tavangar indicated no relevant financial relationships.
Brian Mendoza indicated no relevant financial relationships.
Peter Nguyen indicated no relevant financial relationships.
Jason Samarasena: Cook Medical – Consultant. Medtronic – Advisory Committee/Board Member, Consultant. Neptune Medical – Advisory Committee/Board Member, Consultant. Olympus – Advisory Committee/Board Member, Consultant. Ovesco – Advisory Committee/Board Member, Consultant, Speakers Bureau. SatisfAI – Stock-privately held company. Steris – Advisory Committee/Board Member.
Frances Dang indicated no relevant financial relationships.
Shoujit Banerjee, MD1, Bryant Le, MD1, Andy L. Lin, MD2, Marie Balfour, MD2, Amirali Tavangar, MD2, Brian Mendoza, MD2, Peter H. Nguyen, MD2, Jason Samarasena, MD2, Frances Dang, MD2. P5021 - Duodenum in Distress: A Rare Case of Obstruction From Aortic Aneurysm, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
