Tuesday Poster Session
Category: Small Intestine
P5026 - Olmesartan-Induced Enteropathy Resulting in Hypokalemia-Induced Rhabdomyolysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Irtiqa Fazili, MD
Emory University
Suwanee, GA
Presenting Author(s)
Irtiqa Fazili, MD1, Annie Massart, MD2, Anna Maurer, MSc3
1Emory University, Suwanee, GA; 2Emory University Hospital, Atlanta, GA; 3Emory University School of Medicine, Atlanta, GA
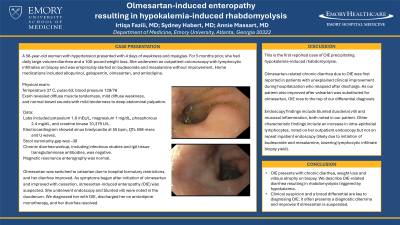
Introduction: Olmesartan-induced enteropathy (OIE) presents with chronic diarrhea, weight loss and villous atrophy on biopsy. We describe OIE-related diarrhea resulting in rhabdomyolysis triggered by hypokalemia.
Case Description/Methods: A 58-year-old female with hypertension presented with 4 days of weakness and myalgias.
For 5 months prior, she had daily large-volume diarrhea and 100-pound weight loss. She underwent colonoscopy with lymphocytic infiltrates on biopsy and was empirically started on budesonide and mesalamine without improvement. Home medications included allopurinol, gabapentin, olmesartan, and amlodipine.
On presentation, blood pressure was 129/76, pulse 63, temperature 37°C, BMI 36.4. She had diffuse muscle tenderness. Labs included potassium 1.6 mEq/L, magnesium 1 mg/dL, phosphorous 2.4 mg/dL, and creatine kinase 10,379 U/L. EKG showed QT prolongation and U waves.
Stool osmolarity gap was –38. Chronic diarrhea workup, including infectious studies and IgA tissue transglutaminase antibodies, was negative. Magnetic resonance enterography was normal. Olmesartan was switched to valsartan due to hospital formulary restrictions, and her diarrhea improved.
As symptoms began after initiation of olmesartan and improved with cessation, OIE was suspected. She underwent endoscopy and blunted villi were noted in the duodenum. We diagnosed her with OIE, discharged her on amlodipine monotherapy, and her diarrhea resolved.
Discussion: This is the first reported case of OIE precipitating hypokalemia-induced rhabdomyolysis.
Olmesartan-related chronic diarrhea due to OIE was first reported in patients with unexplained clinical improvement during hospitalization who relapsed after discharge. As our patient also improved after valsartan was substituted for olmesartan, OIE rose to the top of our differential diagnosis.
Endoscopy findings include blunted duodenal villi and mucosal inflammation, both noted in our patient. Other characteristic findings include increase in intra-epithelial lymphocytes, noted on her outpatient endoscopy but not on repeat inpatient endoscopy (likely due to initiation of budesonide and mesalamine, lowering lymphocytic infiltrate biopsy yield).
Clinical suspicion and a broad differential are key to diagnosing OIE; it often presents a diagnostic dilemma and improves if olmesartan is suspended.
Disclosures:
Irtiqa Fazili, MD1, Annie Massart, MD2, Anna Maurer, MSc3. P5026 - Olmesartan-Induced Enteropathy Resulting in Hypokalemia-Induced Rhabdomyolysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Emory University, Suwanee, GA; 2Emory University Hospital, Atlanta, GA; 3Emory University School of Medicine, Atlanta, GA
Introduction: Olmesartan-induced enteropathy (OIE) presents with chronic diarrhea, weight loss and villous atrophy on biopsy. We describe OIE-related diarrhea resulting in rhabdomyolysis triggered by hypokalemia.
Case Description/Methods: A 58-year-old female with hypertension presented with 4 days of weakness and myalgias.
For 5 months prior, she had daily large-volume diarrhea and 100-pound weight loss. She underwent colonoscopy with lymphocytic infiltrates on biopsy and was empirically started on budesonide and mesalamine without improvement. Home medications included allopurinol, gabapentin, olmesartan, and amlodipine.
On presentation, blood pressure was 129/76, pulse 63, temperature 37°C, BMI 36.4. She had diffuse muscle tenderness. Labs included potassium 1.6 mEq/L, magnesium 1 mg/dL, phosphorous 2.4 mg/dL, and creatine kinase 10,379 U/L. EKG showed QT prolongation and U waves.
Stool osmolarity gap was –38. Chronic diarrhea workup, including infectious studies and IgA tissue transglutaminase antibodies, was negative. Magnetic resonance enterography was normal. Olmesartan was switched to valsartan due to hospital formulary restrictions, and her diarrhea improved.
As symptoms began after initiation of olmesartan and improved with cessation, OIE was suspected. She underwent endoscopy and blunted villi were noted in the duodenum. We diagnosed her with OIE, discharged her on amlodipine monotherapy, and her diarrhea resolved.
Discussion: This is the first reported case of OIE precipitating hypokalemia-induced rhabdomyolysis.
Olmesartan-related chronic diarrhea due to OIE was first reported in patients with unexplained clinical improvement during hospitalization who relapsed after discharge. As our patient also improved after valsartan was substituted for olmesartan, OIE rose to the top of our differential diagnosis.
Endoscopy findings include blunted duodenal villi and mucosal inflammation, both noted in our patient. Other characteristic findings include increase in intra-epithelial lymphocytes, noted on her outpatient endoscopy but not on repeat inpatient endoscopy (likely due to initiation of budesonide and mesalamine, lowering lymphocytic infiltrate biopsy yield).
Clinical suspicion and a broad differential are key to diagnosing OIE; it often presents a diagnostic dilemma and improves if olmesartan is suspended.
Disclosures:
Irtiqa Fazili indicated no relevant financial relationships.
Annie Massart indicated no relevant financial relationships.
Anna Maurer indicated no relevant financial relationships.
Irtiqa Fazili, MD1, Annie Massart, MD2, Anna Maurer, MSc3. P5026 - Olmesartan-Induced Enteropathy Resulting in Hypokalemia-Induced Rhabdomyolysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

