Tuesday Poster Session
Category: Small Intestine
P5029 - Hypereosinophilic Syndrome Manifested as Eosinophilic Jejunitis in a Patient Presenting With Mesenteric Adenitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Kwabena Asafo-Agyei, MBChB
Medical College of Georgia, Augusta University
Augusta, GA
Presenting Author(s)
Kwabena Asafo-Agyei, MBChB1, John Kirkikis, MD2, Dustin Hadley, PA-C2, Angela Barnes, MD, MBChB3, Prince Tano. Djan, MD4
1Medical College of Georgia, Augusta University, Augusta, GA; 2GIS, Shreveport, LA; 3Medical College of Georgia at Augusta University, Augusta, GA; 4Cone Health Alamance, Burlington, NC
Introduction: Hypereosinophilic syndrome (HES) is defined as peripheral absolute eosinophilic count ≥ 1500/μL with or without end-organ damage. Eosinophilic enteritis is a rare disorder with myriad gastrointestinal manifestations, including abdominal pain and bloating, diarrhea, nausea, vomiting, and failure to thrive due to eosinophilic infiltration of the small intestines without other organ involvement and with the exclusion of other etiologies for eosinophilia.
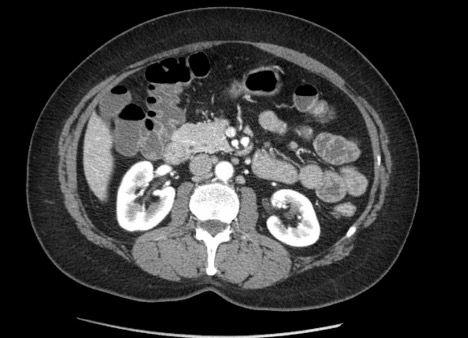
Case Description/Methods: This is a 51-year-old white female with a history of Hashimoto's thyroiditis presented to the emergency department (ED) at an outside facility with severe abdominal pain, bloating, and constipation. She ate sushi a week before her presentation and noted worsening epigastric pain worse with eating afterward, which was associated with nausea but no vomiting. Computed tomography (CT) of the abdomen and pelvis with intravenous contrast revealed some thickening of the jejunum and mesenteric node inflammation, consistent with mesenteric adenitis.
On arrival, laboratory findings included leukocytosis with differential eosinophilia of 19%. The absolute eosinophilia count was 1376 and was increased to 2989 the following day.
CT enterography on admission revealed similar findings (Fig 1).
She had EGD with an enteroscopy, which revealed a normal esophagus, gastritis, and mild inflammation of the jejunum. Multiple biopsies were taken, and pathology showed numerous eosinophils, seen predominantly within the small intestinal fragments lacking Brunner's glands. Eosinophils were seen within crypt epithelium, muscularis mucosa, and lamina propria, focally numbering greater than 100 per high power field. The gastric biopsy revealed gastric mucosa with minimal nonspecific chronic inflammation and no evidence of eosinophilia. The patient was diagnosed with eosinophilic enteritis and referred to an allergy specialist.
The patient was started on mepolizumab after refusing steroid therapy, and absolute eosinophils trended downwards to 163 with the resolution of symptoms.
Discussion: Eosinophilic gastrointestinal disorders (EGID) are often classified under Overlap HES. This disease is restricted to a single organ system accompanied by blood eosinophilia ≥ 1500 109 /L.
Due to the myriad presentations of eosinophilic enteritis, gastroenterologists, radiologists, and internists should have a high suspicion for patients presenting with peripheral eosinophilia without other probable causes to prompt early diagnosis and management of this disease.
Disclosures:
Kwabena Asafo-Agyei, MBChB1, John Kirkikis, MD2, Dustin Hadley, PA-C2, Angela Barnes, MD, MBChB3, Prince Tano. Djan, MD4. P5029 - Hypereosinophilic Syndrome Manifested as Eosinophilic Jejunitis in a Patient Presenting With Mesenteric Adenitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Medical College of Georgia, Augusta University, Augusta, GA; 2GIS, Shreveport, LA; 3Medical College of Georgia at Augusta University, Augusta, GA; 4Cone Health Alamance, Burlington, NC
Introduction: Hypereosinophilic syndrome (HES) is defined as peripheral absolute eosinophilic count ≥ 1500/μL with or without end-organ damage. Eosinophilic enteritis is a rare disorder with myriad gastrointestinal manifestations, including abdominal pain and bloating, diarrhea, nausea, vomiting, and failure to thrive due to eosinophilic infiltration of the small intestines without other organ involvement and with the exclusion of other etiologies for eosinophilia.
Case Description/Methods: This is a 51-year-old white female with a history of Hashimoto's thyroiditis presented to the emergency department (ED) at an outside facility with severe abdominal pain, bloating, and constipation. She ate sushi a week before her presentation and noted worsening epigastric pain worse with eating afterward, which was associated with nausea but no vomiting. Computed tomography (CT) of the abdomen and pelvis with intravenous contrast revealed some thickening of the jejunum and mesenteric node inflammation, consistent with mesenteric adenitis.
On arrival, laboratory findings included leukocytosis with differential eosinophilia of 19%. The absolute eosinophilia count was 1376 and was increased to 2989 the following day.
CT enterography on admission revealed similar findings (Fig 1).
She had EGD with an enteroscopy, which revealed a normal esophagus, gastritis, and mild inflammation of the jejunum. Multiple biopsies were taken, and pathology showed numerous eosinophils, seen predominantly within the small intestinal fragments lacking Brunner's glands. Eosinophils were seen within crypt epithelium, muscularis mucosa, and lamina propria, focally numbering greater than 100 per high power field. The gastric biopsy revealed gastric mucosa with minimal nonspecific chronic inflammation and no evidence of eosinophilia. The patient was diagnosed with eosinophilic enteritis and referred to an allergy specialist.
The patient was started on mepolizumab after refusing steroid therapy, and absolute eosinophils trended downwards to 163 with the resolution of symptoms.
Discussion: Eosinophilic gastrointestinal disorders (EGID) are often classified under Overlap HES. This disease is restricted to a single organ system accompanied by blood eosinophilia ≥ 1500 109 /L.
Due to the myriad presentations of eosinophilic enteritis, gastroenterologists, radiologists, and internists should have a high suspicion for patients presenting with peripheral eosinophilia without other probable causes to prompt early diagnosis and management of this disease.
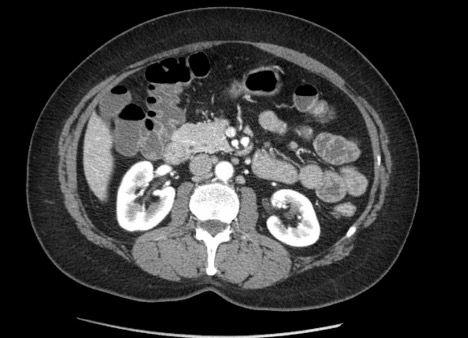
Figure: CT ENTEROGRAPHY
Disclosures:
Kwabena Asafo-Agyei indicated no relevant financial relationships.
John Kirkikis indicated no relevant financial relationships.
Dustin Hadley indicated no relevant financial relationships.
Angela Barnes indicated no relevant financial relationships.
Prince Djan indicated no relevant financial relationships.
Kwabena Asafo-Agyei, MBChB1, John Kirkikis, MD2, Dustin Hadley, PA-C2, Angela Barnes, MD, MBChB3, Prince Tano. Djan, MD4. P5029 - Hypereosinophilic Syndrome Manifested as Eosinophilic Jejunitis in a Patient Presenting With Mesenteric Adenitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
