Tuesday Poster Session
Category: Stomach
P5059 - Gastrostomy Among COVID-19 Positive Patients: Did the Procedure Method Influence Complications and Mortality?
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- RV
Renuka Verma, MD
University of Nevada
Las Vegas, NV
Presenting Author(s)
Renuka Verma, MD1, Kyaw Min Tun, DO2, Hemamalini Sakthivel, MD3, Kamleshun Ramphul, MD4, Banreet Dhindsa, MD5, Douglas Adler, MD6
1University of Nevada, Las Vegas, NV; 2Creighton University School of Medicine, Las Vegas, NV; 3One Brooklyn Health-Interfaith Medical Center, New York, NY; 4Independent Researcher, Triolet, Pamplemousses, Mauritius; 5NYU Grossman School of Medicine, New York, NY; 6Center for Advanced Therapeutic (CATE), Centura Health, Porter Adventist Hospital, Peak Gastroenterology, Denver, CO
Introduction: A recent study found a significant rise in procedures for feeding tube placement during the first year of the COVID-19 pandemic in the United States. To date, there are no data evaluating the use of such procedures among COVID-19 patients. Via our retrospective study, we aim to evaluate the differences in characteristics and mortality among COVID-19 patients undergoing gastrostomy by surgery (open)(SG), Interventional Radiology (IR)(IRG), and gastroenterology team(Percutaneous endoscopic gastrostomy, PEG).
Methods: Adults (ages ≥18 years) with a primary diagnosis of COVID-19 were studied using the 2020-2021 National Inpatient Sample. We excluded cases before April 2020. The age, Charlson Comorbidity Index (CCI) score, and length of stay(LOS, days) between SG, IRG, and PEG patients were compared. Various complications and deaths were evaluated using multivariable regression analysis.
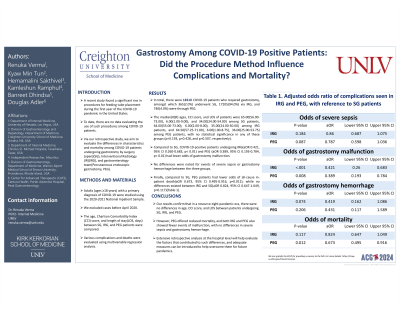
Results: In total, there were 18310 COVID-19 patients who required gastrostomy, amongst which 365(2.0%) underwent SG, 17205(94.0%) via IRG, and 740(4.0%) were through PEG. The median(IQR) ages, CCI score, and LOS of patients were 65.00(56.00-73.00), 6.00(1.00-9.00), and 34.00(24.00-54.00) among SG patients, 64.00(55.00-73.00), 6.00(2.00-8.00), 35.00(24.00-50.00) among IRG patients, and 64.50(57.25-71.00), 6.00(1.00-8.75), 36.00(25.00-53.75) among PEG patients, with no statistical significance in any of these groups (p=0.193, p=0.428, and p=0.507, respectively). Compared to SG, COVID-19-positive patients undergoing IQR(aOR 0.421, 95% CI 0.260-0.683, p< 0.01) and PEG (aOR 0.389, 95% CI 0.193-0.784, p< 0.01) had lower odds of gastrostomy malfunction. No differences were noted for events of severe sepsis or gastrostomy hemorrhage between the three groups. Finally, compared to SG, PEG patients had lower odds of all-cause in-patient death(aOR 0.673, 95% CI 0.495-0.916, p=0.012), while no differences existed between IRG and SG(aOR 0.824, 95% CI 0.647-1.049, p=0.117)(Table 1).
Discussion: Our results confirm that in a resource-tight pandemic era, there were no differences in age, CCI score, and LOS between patients undergoing SG, IRG, and PEG. However, PEG offered reduced mortality, and both IRQ and PEG also showed fewer events of malfunction, with no differences in severe sepsis and gastrostomy hemorrhage. Extensive retrospective analysis at the hospital level will help evaluate the factors that contributed to such differences, and adequate measures can be introduced to help overcome them for future pandemics.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Renuka Verma, MD1, Kyaw Min Tun, DO2, Hemamalini Sakthivel, MD3, Kamleshun Ramphul, MD4, Banreet Dhindsa, MD5, Douglas Adler, MD6. P5059 - Gastrostomy Among COVID-19 Positive Patients: Did the Procedure Method Influence Complications and Mortality?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Nevada, Las Vegas, NV; 2Creighton University School of Medicine, Las Vegas, NV; 3One Brooklyn Health-Interfaith Medical Center, New York, NY; 4Independent Researcher, Triolet, Pamplemousses, Mauritius; 5NYU Grossman School of Medicine, New York, NY; 6Center for Advanced Therapeutic (CATE), Centura Health, Porter Adventist Hospital, Peak Gastroenterology, Denver, CO
Introduction: A recent study found a significant rise in procedures for feeding tube placement during the first year of the COVID-19 pandemic in the United States. To date, there are no data evaluating the use of such procedures among COVID-19 patients. Via our retrospective study, we aim to evaluate the differences in characteristics and mortality among COVID-19 patients undergoing gastrostomy by surgery (open)(SG), Interventional Radiology (IR)(IRG), and gastroenterology team(Percutaneous endoscopic gastrostomy, PEG).
Methods: Adults (ages ≥18 years) with a primary diagnosis of COVID-19 were studied using the 2020-2021 National Inpatient Sample. We excluded cases before April 2020. The age, Charlson Comorbidity Index (CCI) score, and length of stay(LOS, days) between SG, IRG, and PEG patients were compared. Various complications and deaths were evaluated using multivariable regression analysis.
Results: In total, there were 18310 COVID-19 patients who required gastrostomy, amongst which 365(2.0%) underwent SG, 17205(94.0%) via IRG, and 740(4.0%) were through PEG. The median(IQR) ages, CCI score, and LOS of patients were 65.00(56.00-73.00), 6.00(1.00-9.00), and 34.00(24.00-54.00) among SG patients, 64.00(55.00-73.00), 6.00(2.00-8.00), 35.00(24.00-50.00) among IRG patients, and 64.50(57.25-71.00), 6.00(1.00-8.75), 36.00(25.00-53.75) among PEG patients, with no statistical significance in any of these groups (p=0.193, p=0.428, and p=0.507, respectively). Compared to SG, COVID-19-positive patients undergoing IQR(aOR 0.421, 95% CI 0.260-0.683, p< 0.01) and PEG (aOR 0.389, 95% CI 0.193-0.784, p< 0.01) had lower odds of gastrostomy malfunction. No differences were noted for events of severe sepsis or gastrostomy hemorrhage between the three groups. Finally, compared to SG, PEG patients had lower odds of all-cause in-patient death(aOR 0.673, 95% CI 0.495-0.916, p=0.012), while no differences existed between IRG and SG(aOR 0.824, 95% CI 0.647-1.049, p=0.117)(Table 1).
Discussion: Our results confirm that in a resource-tight pandemic era, there were no differences in age, CCI score, and LOS between patients undergoing SG, IRG, and PEG. However, PEG offered reduced mortality, and both IRQ and PEG also showed fewer events of malfunction, with no differences in severe sepsis and gastrostomy hemorrhage. Extensive retrospective analysis at the hospital level will help evaluate the factors that contributed to such differences, and adequate measures can be introduced to help overcome them for future pandemics.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Renuka Verma indicated no relevant financial relationships.
Kyaw Min Tun indicated no relevant financial relationships.
Hemamalini Sakthivel indicated no relevant financial relationships.
Kamleshun Ramphul indicated no relevant financial relationships.
Banreet Dhindsa indicated no relevant financial relationships.
Douglas Adler: Boston Scientific and Micro Tech. – Consultant.
Renuka Verma, MD1, Kyaw Min Tun, DO2, Hemamalini Sakthivel, MD3, Kamleshun Ramphul, MD4, Banreet Dhindsa, MD5, Douglas Adler, MD6. P5059 - Gastrostomy Among COVID-19 Positive Patients: Did the Procedure Method Influence Complications and Mortality?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
