Tuesday Poster Session
Category: Stomach
P5092 - Endoscopic Management of Gastric Outlet Obstruction Using Hypertonic Saline Solution
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- RC
Ronan Calibuso, MD
Jersey City, NJ
Presenting Author(s)
Ronan Calibuso, MD1, Deva Christine T. Tojong, MD2, Gomathy A. Nageswaran, MBBS3, Loc Ton, MD4, John Erikson Yap, MD, MBA, FACG5
1Jersey City, NJ; 2Medical College of Georgia at Augusta University, Augusta, GA; 3University of Arkansas for Medical Sciences, Little Rock, AR; 4Kaiser Permanente, South Sacramento, CA; 5Metrodora Institute, West Valley City, UT
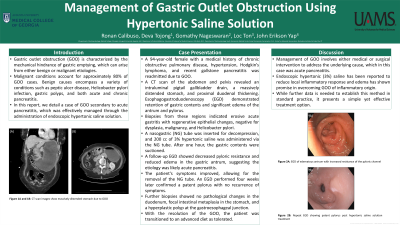
Introduction: Gastric outlet obstruction (GOO) is characterized by the mechanical hindrance of gastric emptying, which can arise from either benign or malignant etiologies. Malignant conditions account for approximately 80% of GOO cases. Benign causes encompass a variety of conditions such as peptic ulcer disease, Helicobacter pylori infection, gastric polyps, and both acute and chronic pancreatitis. In this report, we detail a case of GOO secondary to acute pancreatitis, which was effectively managed through the administration of endoscopic hypertonic saline solution.
Case Description/Methods: A 94-year-old female with a medical history of chronic obstructive pulmonary disease, hypertension, Hodgkin’s lymphoma, and recent gallstone pancreatitis was readmitted due to GOO. A CT scan of the abdomen and pelvis revealed an intraluminal pigtail gallbladder drain, a massively distended stomach, and proximal duodenal thickening. Esophagogastroduodenoscopy (EGD) demonstrated retention of gastric contents and significant edema of the antrum and pylorus. Biopsies from these regions indicated erosive acute gastritis with regenerative epithelial changes, negative for dysplasia, malignancy, and Helicobacter pylori. A nasogastric (NG) tube was inserted for decompression, and 200 cc of 3% hypertonic saline was administered via the NG tube. After one hour, the gastric contents were suctioned. A follow-up EGD showed decreased pyloric resistance and reduced edema in the gastric antrum, suggesting the etiology was likely acute pancreatitis. The patient's symptoms improved, allowing for the removal of the NG tube. An EGD performed four weeks later confirmed a patent pylorus with no recurrence of symptoms. Further biopsies showed no pathological changes in the duodenum, focal intestinal metaplasia in the stomach, and a hyperplastic polyp at the gastroesophageal junction. With the resolution of the GOO, the patient was transitioned to an advanced diet as tolerated.
Discussion: Management of GOO involves either medical or surgical intervention to address the underlying cause, which in this case was acute pancreatitis. Endoscopic hypertonic (3%) saline has been reported to reduce local inflammatory response and edema has shown promise in overcoming GOO of inflammatory origin. While further data is needed to establish this method in standard practice, it presents a simple yet effective treatment option.
Disclosures:
Ronan Calibuso, MD1, Deva Christine T. Tojong, MD2, Gomathy A. Nageswaran, MBBS3, Loc Ton, MD4, John Erikson Yap, MD, MBA, FACG5. P5092 - Endoscopic Management of Gastric Outlet Obstruction Using Hypertonic Saline Solution, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jersey City, NJ; 2Medical College of Georgia at Augusta University, Augusta, GA; 3University of Arkansas for Medical Sciences, Little Rock, AR; 4Kaiser Permanente, South Sacramento, CA; 5Metrodora Institute, West Valley City, UT
Introduction: Gastric outlet obstruction (GOO) is characterized by the mechanical hindrance of gastric emptying, which can arise from either benign or malignant etiologies. Malignant conditions account for approximately 80% of GOO cases. Benign causes encompass a variety of conditions such as peptic ulcer disease, Helicobacter pylori infection, gastric polyps, and both acute and chronic pancreatitis. In this report, we detail a case of GOO secondary to acute pancreatitis, which was effectively managed through the administration of endoscopic hypertonic saline solution.
Case Description/Methods: A 94-year-old female with a medical history of chronic obstructive pulmonary disease, hypertension, Hodgkin’s lymphoma, and recent gallstone pancreatitis was readmitted due to GOO. A CT scan of the abdomen and pelvis revealed an intraluminal pigtail gallbladder drain, a massively distended stomach, and proximal duodenal thickening. Esophagogastroduodenoscopy (EGD) demonstrated retention of gastric contents and significant edema of the antrum and pylorus. Biopsies from these regions indicated erosive acute gastritis with regenerative epithelial changes, negative for dysplasia, malignancy, and Helicobacter pylori. A nasogastric (NG) tube was inserted for decompression, and 200 cc of 3% hypertonic saline was administered via the NG tube. After one hour, the gastric contents were suctioned. A follow-up EGD showed decreased pyloric resistance and reduced edema in the gastric antrum, suggesting the etiology was likely acute pancreatitis. The patient's symptoms improved, allowing for the removal of the NG tube. An EGD performed four weeks later confirmed a patent pylorus with no recurrence of symptoms. Further biopsies showed no pathological changes in the duodenum, focal intestinal metaplasia in the stomach, and a hyperplastic polyp at the gastroesophageal junction. With the resolution of the GOO, the patient was transitioned to an advanced diet as tolerated.
Discussion: Management of GOO involves either medical or surgical intervention to address the underlying cause, which in this case was acute pancreatitis. Endoscopic hypertonic (3%) saline has been reported to reduce local inflammatory response and edema has shown promise in overcoming GOO of inflammatory origin. While further data is needed to establish this method in standard practice, it presents a simple yet effective treatment option.
Disclosures:
Ronan Calibuso indicated no relevant financial relationships.
Deva Christine Tojong indicated no relevant financial relationships.
Gomathy Nageswaran indicated no relevant financial relationships.
Loc Ton indicated no relevant financial relationships.
John Erikson Yap indicated no relevant financial relationships.
Ronan Calibuso, MD1, Deva Christine T. Tojong, MD2, Gomathy A. Nageswaran, MBBS3, Loc Ton, MD4, John Erikson Yap, MD, MBA, FACG5. P5092 - Endoscopic Management of Gastric Outlet Obstruction Using Hypertonic Saline Solution, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
