Tuesday Poster Session
Category: Stomach
P5093 - More Than Just Bloating: A Case of Gastric Pneumatosis in a Patient With Celiac Artery Occlusion and Diabetic Ketoacidosis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Arvin Jeremy Tan, MD
University of Hawaii, John A. Burns School of Medicine
Honolulu, HI
Presenting Author(s)
Arvin Jeremy Tan, MD1, Jennie Zhang, MD2, Vinay Rao, MD2, Raymond Janowski, MD2, Marie L.. Borum, MD, MPH, FACG2, Samuel A.. Schueler, MD2
1University of Hawaii, John A. Burns School of Medicine, Honolulu, HI; 2George Washington University School of Medicine and Health Sciences, Washington, DC
Introduction: Gastric pneumatosis is a rare radiographic entity characterized by gas within the stomach wall. It is part of a spectrum of intestinal pneumatosis with the stomach being least commonly affected. Clinically, it is related to gastric emphysema which has a good prognosis, or emphysematous gastritis with a mortality rate of at least 60%. Here, we present a patient with gastric pneumatosis in the setting of diabetic ketoacidosis (DKA) and celiac artery occlusion.
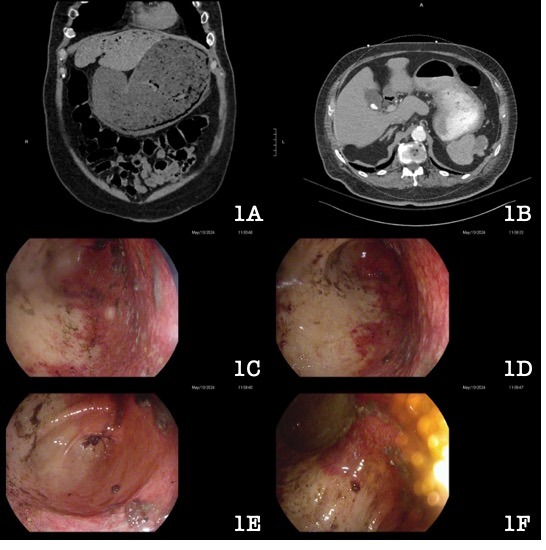
Case Description/Methods: A 77-year-old male with peripheral arterial disease, prior DVT and splenic infarction, atrial fibrillation, hypertension, and gout presented with abdominal pain, nausea, vomiting, and diarrhea. At an outside hospital, he was treated with prednisone for Bell’s Palsy and found to be in DKA. Computed tomography (CT) revealed gastric pneumatosis with portal venous gas (Image 1A) prompting transfer to our institution. He subsequently developed bloody nasogastric output, melena, and hemoglobin drop from 10 to 8 g/dL. Esophagogastroduodenoscopy revealed a sharply demarcated area of pallor involving the lesser curvature and erythematous mucosa in the greater curvature suggesting ischemia (Image 1C-1F). CT angiography revealed an occluded celiac artery with collateral filling through the gastroduodenal artery (Image 1B). Mesenteric angiogram revealed perfusion to the stomach from the right gastric artery and epiploic branches. He underwent aorto-hepatic bypass surgery with subsequent clinical improvement.
Discussion: Gastric pneumatosis can result from local or systemic hypoperfusion, disruption of the gastric mucosa, dissection of mediastinal air, or infection by gas-producing organisms. The varied mechanisms are not mutually exclusive and may occur together. Elevated lactate and creatinine are associated with increased mortality. Treatment is based on the etiology with surgery reserved for severe cases. The cause in our patient was likely multifactorial due to underlying chronic hypoperfusion and mucosal disruption secondary to vomiting in the setting of DKA. He underwent reperfusion surgery with clinical improvement. This rare finding should prompt clinicians to expedite identifying and treating the underlying etiology given the potential for morbidity and mortality.
Disclosures:
Arvin Jeremy Tan, MD1, Jennie Zhang, MD2, Vinay Rao, MD2, Raymond Janowski, MD2, Marie L.. Borum, MD, MPH, FACG2, Samuel A.. Schueler, MD2. P5093 - More Than Just Bloating: A Case of Gastric Pneumatosis in a Patient With Celiac Artery Occlusion and Diabetic Ketoacidosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Hawaii, John A. Burns School of Medicine, Honolulu, HI; 2George Washington University School of Medicine and Health Sciences, Washington, DC
Introduction: Gastric pneumatosis is a rare radiographic entity characterized by gas within the stomach wall. It is part of a spectrum of intestinal pneumatosis with the stomach being least commonly affected. Clinically, it is related to gastric emphysema which has a good prognosis, or emphysematous gastritis with a mortality rate of at least 60%. Here, we present a patient with gastric pneumatosis in the setting of diabetic ketoacidosis (DKA) and celiac artery occlusion.
Case Description/Methods: A 77-year-old male with peripheral arterial disease, prior DVT and splenic infarction, atrial fibrillation, hypertension, and gout presented with abdominal pain, nausea, vomiting, and diarrhea. At an outside hospital, he was treated with prednisone for Bell’s Palsy and found to be in DKA. Computed tomography (CT) revealed gastric pneumatosis with portal venous gas (Image 1A) prompting transfer to our institution. He subsequently developed bloody nasogastric output, melena, and hemoglobin drop from 10 to 8 g/dL. Esophagogastroduodenoscopy revealed a sharply demarcated area of pallor involving the lesser curvature and erythematous mucosa in the greater curvature suggesting ischemia (Image 1C-1F). CT angiography revealed an occluded celiac artery with collateral filling through the gastroduodenal artery (Image 1B). Mesenteric angiogram revealed perfusion to the stomach from the right gastric artery and epiploic branches. He underwent aorto-hepatic bypass surgery with subsequent clinical improvement.
Discussion: Gastric pneumatosis can result from local or systemic hypoperfusion, disruption of the gastric mucosa, dissection of mediastinal air, or infection by gas-producing organisms. The varied mechanisms are not mutually exclusive and may occur together. Elevated lactate and creatinine are associated with increased mortality. Treatment is based on the etiology with surgery reserved for severe cases. The cause in our patient was likely multifactorial due to underlying chronic hypoperfusion and mucosal disruption secondary to vomiting in the setting of DKA. He underwent reperfusion surgery with clinical improvement. This rare finding should prompt clinicians to expedite identifying and treating the underlying etiology given the potential for morbidity and mortality.
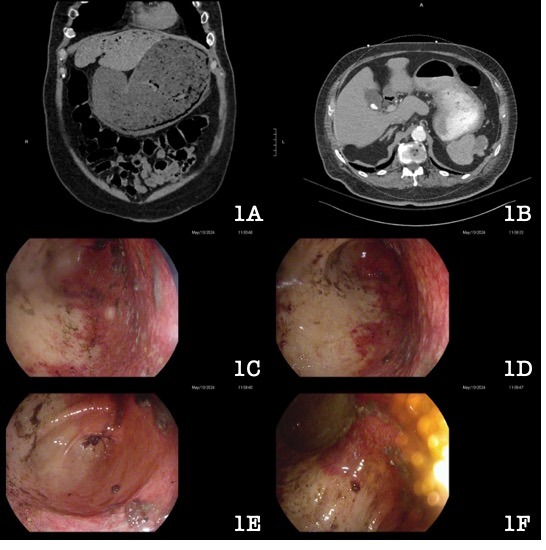
Figure: 1A: CT imaging of the abdomen and pelvis showing a distended stomach with wall-thickening gastric pneumatosis.
1B: CT angiogram showing non-opacification of the celiac artery with severe atherosclerotic calcifications at the ostium.
1C-1F: Endoscopic images showing pallor of the lesser curvature and diffuse erythema of the greater curvature consistent with ischemia (1C-1E), and the incisura in retroflexion (1F).
1B: CT angiogram showing non-opacification of the celiac artery with severe atherosclerotic calcifications at the ostium.
1C-1F: Endoscopic images showing pallor of the lesser curvature and diffuse erythema of the greater curvature consistent with ischemia (1C-1E), and the incisura in retroflexion (1F).
Disclosures:
Arvin Jeremy Tan indicated no relevant financial relationships.
Jennie Zhang indicated no relevant financial relationships.
Vinay Rao indicated no relevant financial relationships.
Raymond Janowski indicated no relevant financial relationships.
Marie Borum: Takeda Pharmaceuticals – Consultant, Speakers Bureau.
Samuel Schueler indicated no relevant financial relationships.
Arvin Jeremy Tan, MD1, Jennie Zhang, MD2, Vinay Rao, MD2, Raymond Janowski, MD2, Marie L.. Borum, MD, MPH, FACG2, Samuel A.. Schueler, MD2. P5093 - More Than Just Bloating: A Case of Gastric Pneumatosis in a Patient With Celiac Artery Occlusion and Diabetic Ketoacidosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
