Tuesday Poster Session
Category: Stomach
P5097 - Immune Checkpoint Inhibitor-Induced Hemorrhagic Gastritis: Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio

Amelia A. Tochtrop
Mercer University School of Medicine
Carrollton, GA
Presenting Author(s)
Amelia A. Tochtrop, 1, Samantha Johnson, 1, Katherine Wells, 1, Janine Burgher-Jones, MD2
1Mercer University School of Medicine, Columbus, GA; 2Piedmont Columbus Midtown, Columbus, GA
Introduction: Immune checkpoint inhibitors (ICIs) are powerful anti-neoplastic monoclonal antibodies that carry an associated risk of causing organ toxicity, known as immune-related adverse events (irAEs). Gastrointestinal irAEs (GI-irAEs) can cause potentially severe symptoms that often require interruption of cancer treatment. Colitis is a well-known GI-irAE, however, isolated gastric involvement is rare, with a reported incidence of less than 1.5%. Current clinical guidelines do not include explicit guidance regarding the grading and management of ICI gastritis in the absence of diarrhea or colitis. This case report aims to supplement the current data on the clinical manifestations, endoscopic evaluation and response to treatments in a patient with isolated ICI-gastritis.
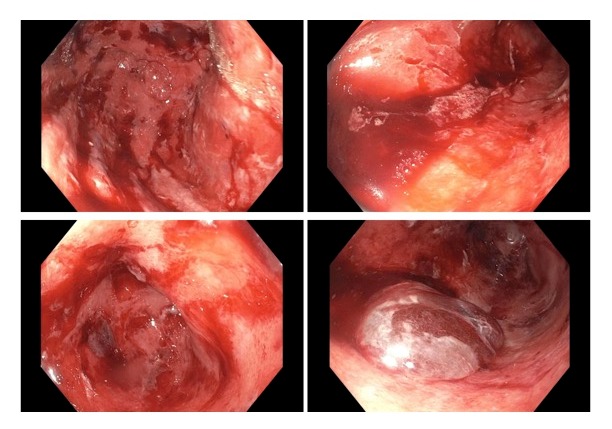
Case Description/Methods: A 52 year old man with metastatic melanoma presented to the ED with epigastric pain and nausea five days after completing his ninth cycle of combined therapy with pembrolizumab and ipilimumab. He was given famotidine and ondansetron for his symptoms but returned two days later for symptom progression. Immunotherapy was held and he began metoclopramide and omeprazole. Five days later he returned with persistent symptoms. Upper endoscopy with biopsy revealed severe hemorrhagic, sloughing gastritis with erosions, ulcerations, and friable mucosa (figure 1). Sucralfate and cyproheptadine were started but he returned one week later for nausea and vomiting with hematemesis and significant weight loss. The gastric biopsy confirmed the presence of fibrinopurulent exudate, atrophic glands and apoptosis, consistent with ICI gastritis. Treatment with oral prednisolone was initiated and the patient reported complete resolution of symptoms one week later. Immunotherapy was held for five weeks during steroid taper. Ultimately, alternate immunotherapy with nivolumab was initiated without gastritis recurrence.
Discussion: With ICIs becoming the mainstay for managing malignancies there will be an increased frequency of presentations for irAEs. Therefore, awareness of the clinical features, diagnostic strategies and management of these toxicities is imperative. There should be a low threshold for performing endoscopy with biopsy in patients undergoing ICI therapy that present with gastritis symptoms. High-dose steroids are effective for managing ICI gastritis, but care should be given to ensure adverse effects of steroids on the GI system are mitigated with concurrent use of proton pump inhibitors.
Disclosures:
Amelia A. Tochtrop, 1, Samantha Johnson, 1, Katherine Wells, 1, Janine Burgher-Jones, MD2. P5097 - Immune Checkpoint Inhibitor-Induced Hemorrhagic Gastritis: Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mercer University School of Medicine, Columbus, GA; 2Piedmont Columbus Midtown, Columbus, GA
Introduction: Immune checkpoint inhibitors (ICIs) are powerful anti-neoplastic monoclonal antibodies that carry an associated risk of causing organ toxicity, known as immune-related adverse events (irAEs). Gastrointestinal irAEs (GI-irAEs) can cause potentially severe symptoms that often require interruption of cancer treatment. Colitis is a well-known GI-irAE, however, isolated gastric involvement is rare, with a reported incidence of less than 1.5%. Current clinical guidelines do not include explicit guidance regarding the grading and management of ICI gastritis in the absence of diarrhea or colitis. This case report aims to supplement the current data on the clinical manifestations, endoscopic evaluation and response to treatments in a patient with isolated ICI-gastritis.
Case Description/Methods: A 52 year old man with metastatic melanoma presented to the ED with epigastric pain and nausea five days after completing his ninth cycle of combined therapy with pembrolizumab and ipilimumab. He was given famotidine and ondansetron for his symptoms but returned two days later for symptom progression. Immunotherapy was held and he began metoclopramide and omeprazole. Five days later he returned with persistent symptoms. Upper endoscopy with biopsy revealed severe hemorrhagic, sloughing gastritis with erosions, ulcerations, and friable mucosa (figure 1). Sucralfate and cyproheptadine were started but he returned one week later for nausea and vomiting with hematemesis and significant weight loss. The gastric biopsy confirmed the presence of fibrinopurulent exudate, atrophic glands and apoptosis, consistent with ICI gastritis. Treatment with oral prednisolone was initiated and the patient reported complete resolution of symptoms one week later. Immunotherapy was held for five weeks during steroid taper. Ultimately, alternate immunotherapy with nivolumab was initiated without gastritis recurrence.
Discussion: With ICIs becoming the mainstay for managing malignancies there will be an increased frequency of presentations for irAEs. Therefore, awareness of the clinical features, diagnostic strategies and management of these toxicities is imperative. There should be a low threshold for performing endoscopy with biopsy in patients undergoing ICI therapy that present with gastritis symptoms. High-dose steroids are effective for managing ICI gastritis, but care should be given to ensure adverse effects of steroids on the GI system are mitigated with concurrent use of proton pump inhibitors.
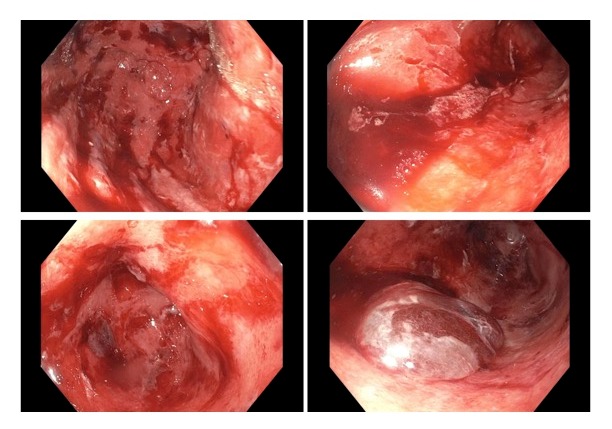
Figure: EGD images showing hemorrhagic, sloughing gastritis with erosions, ulcerations, and friable mucosa throughout the stomach. EGD - esophagogastroduodenoscopy.
Disclosures:
Amelia Tochtrop indicated no relevant financial relationships.
Samantha Johnson indicated no relevant financial relationships.
Katherine Wells indicated no relevant financial relationships.
Janine Burgher-Jones indicated no relevant financial relationships.
Amelia A. Tochtrop, 1, Samantha Johnson, 1, Katherine Wells, 1, Janine Burgher-Jones, MD2. P5097 - Immune Checkpoint Inhibitor-Induced Hemorrhagic Gastritis: Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
