Tuesday Poster Session
Category: Stomach
P5098 - Sarcina Ventriculi: A Rare Cause of Gastric Ulceration
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- TH
Tricia Hengehold, MD
The Ohio State University Wexner Medical Center
Cincinnati, OH
Presenting Author(s)
Tricia Hengehold, MD1, Adam Spandorfer, MD2, Jacob Skeans, MD3
1The Ohio State University Wexner Medical Center, Columbus, OH; 2The Ohio State University College of Medicine, Columbus, OH; 3The Ohio State University, Columbus, OH
Introduction: Gastric ulcers are caused by disruption of the mucosal lining of the stomach with clinical presentation typically involving post-prandial epigastric pain. The most common causes are H. pylori and NSAIDs, and lesser common etiologies include malignancy, ischemia, stress, chemotherapy/radiation, or Crohn’s disease. A rare cause is Sarcina ventriculi, which can lead to gastric ischemic ulcers and if untreated, can progress to gastric perforation.
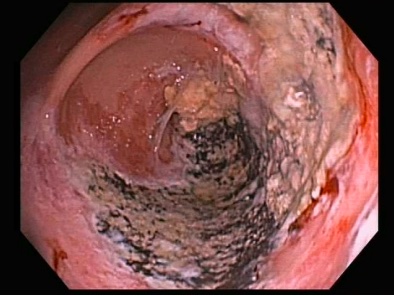
Case Description/Methods: A 60 y/o M w/ PMH of ESRD on hemodialysis and hypertension presented to the hospital with dyspnea. Upon arrival to the hospital, he was noted to have pulmonary edema that was caused by hypertensive emergency that required IV nitroglycerin drip. He also reported a 3-year history of abdominal pain that occurred with eating. He denied any overt bleeding. Labs were significant for hemoglobin of 6.5 g/dL. Due to significant anemia and abdominal pain, an EGD was performed after stabilization. A large necrotic ulcer occupying about 40% of the gastric antrum was seen with distinct borders concerning ischemia without evidence of perforation. Food in the stomach was also noted. Abdominal CT angiogram showed chronic, scattered arterial wall calcifications without occlusions. Biopsies showed gram positive cocci consistent with Sarcina as well as rare luminal fungal yeasts. He was treated with ciprofloxacin and metronidazole for 7 days along with high dose PPI. EGD two months later was notable for healing mucosa with a much smaller clean based ulcer.
Discussion: This patient presented with hypertensive emergency with a history of chronic abdominal pain. The EGD was significant for a necrotic ulcer at risk for gastric perforation. Although hypertensive emergency (and to a lesser extent luminal fungal organisms) likely contributed, Sarcina is a rare finding within ischemic ulcerations that are worrisome for an increased perforation risk. This uncommon gram positive organism, associated with gastroparesis, can live in a low pH environment. Veterinary literature reports it to be a source of gastric dilation and livestock deaths. Sarcina can lead to stomach pain, gastric ulcers, gastric emphysema and ultimately to gastric perforation if untreated. This patient had no known gastroparesis but had food in his stomach despite being NPO the day of procedure. EGD with biopsy lead to the identification of this bacteria in a severely ill patient at risk for perforation. Appropriate antibiotic therapy, along with prolonged PPI use lead to mucosal healing.
Disclosures:
Tricia Hengehold, MD1, Adam Spandorfer, MD2, Jacob Skeans, MD3. P5098 - Sarcina Ventriculi: A Rare Cause of Gastric Ulceration, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The Ohio State University Wexner Medical Center, Columbus, OH; 2The Ohio State University College of Medicine, Columbus, OH; 3The Ohio State University, Columbus, OH
Introduction: Gastric ulcers are caused by disruption of the mucosal lining of the stomach with clinical presentation typically involving post-prandial epigastric pain. The most common causes are H. pylori and NSAIDs, and lesser common etiologies include malignancy, ischemia, stress, chemotherapy/radiation, or Crohn’s disease. A rare cause is Sarcina ventriculi, which can lead to gastric ischemic ulcers and if untreated, can progress to gastric perforation.
Case Description/Methods: A 60 y/o M w/ PMH of ESRD on hemodialysis and hypertension presented to the hospital with dyspnea. Upon arrival to the hospital, he was noted to have pulmonary edema that was caused by hypertensive emergency that required IV nitroglycerin drip. He also reported a 3-year history of abdominal pain that occurred with eating. He denied any overt bleeding. Labs were significant for hemoglobin of 6.5 g/dL. Due to significant anemia and abdominal pain, an EGD was performed after stabilization. A large necrotic ulcer occupying about 40% of the gastric antrum was seen with distinct borders concerning ischemia without evidence of perforation. Food in the stomach was also noted. Abdominal CT angiogram showed chronic, scattered arterial wall calcifications without occlusions. Biopsies showed gram positive cocci consistent with Sarcina as well as rare luminal fungal yeasts. He was treated with ciprofloxacin and metronidazole for 7 days along with high dose PPI. EGD two months later was notable for healing mucosa with a much smaller clean based ulcer.
Discussion: This patient presented with hypertensive emergency with a history of chronic abdominal pain. The EGD was significant for a necrotic ulcer at risk for gastric perforation. Although hypertensive emergency (and to a lesser extent luminal fungal organisms) likely contributed, Sarcina is a rare finding within ischemic ulcerations that are worrisome for an increased perforation risk. This uncommon gram positive organism, associated with gastroparesis, can live in a low pH environment. Veterinary literature reports it to be a source of gastric dilation and livestock deaths. Sarcina can lead to stomach pain, gastric ulcers, gastric emphysema and ultimately to gastric perforation if untreated. This patient had no known gastroparesis but had food in his stomach despite being NPO the day of procedure. EGD with biopsy lead to the identification of this bacteria in a severely ill patient at risk for perforation. Appropriate antibiotic therapy, along with prolonged PPI use lead to mucosal healing.
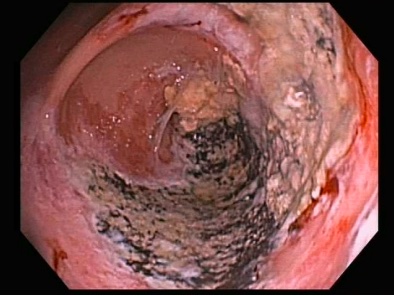
Figure: The endoscopic picture of necrotic appearing ulcerated gastric mucosa with food residue noted.
Disclosures:
Tricia Hengehold indicated no relevant financial relationships.
Adam Spandorfer indicated no relevant financial relationships.
Jacob Skeans indicated no relevant financial relationships.
Tricia Hengehold, MD1, Adam Spandorfer, MD2, Jacob Skeans, MD3. P5098 - Sarcina Ventriculi: A Rare Cause of Gastric Ulceration, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
