Tuesday Poster Session
Category: Stomach
P5100 - Where Did The Balloon Go? A Case of Small Bowel Obstruction Caused by a Displaced Intragastric Balloon
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mena Saad, DO
Riverside University Health System
Moreno Valley, CA
Presenting Author(s)
Mena Saad, DO1, Danyal O. Imam, MBBS1, Jun Song, MD2, Harold J. Duarte, MD3, Emily Lin, MD2, Gunnar Wolfe, MD1, Jee Hoon Song, MD2, Christopher Bent, MD1, Wichit Srikureja, MD1, David X. Liu, MD1, John Agapian, MD1, Steve Serrao, MD1
1Riverside University Health System, Moreno Valley, CA; 2Loma Linda University Medical Center, Loma Linda, CA; 3Loma Linda University Health, Loma Linda, CA
Introduction: With the increasing prevalence of obesity in the United States, the intragastric balloon is a minimally invasive option that works by promoting the feeling of satiation. Intestinal obstruction with migration of the balloon remains a rare but serious complication of intragastric balloon. The risk is increased with prolonged use of intragastric balloons due to the risk of balloon deflation and migration throughout the small and large bowel. We present a case of a small bowel obstruction secondary to a migrated intragastric balloon that was managed endoscopically.
Case Description/Methods: The patient is a 43-year-old male with a past medical history significant for an intragastric balloon placed 2 years ago who presents with epigastric abdominal pain, nausea, and vomiting for 3 days prior to admission. On arrival, he was tachycardic but vital signs were otherwise normal. Laboratory findings were significant for lactate of 3.32 and white blood cell count of 7.2. CT of the abdomen and pelvis showed dilated loops of small bowel with air-fluid levels, mild sigmoid diverticulosis, and an impacted intragastric balloon in the distal ileum. Gastroenterology and Surgery were consulted for the removal of the impacted intragastric balloon. A joint decision was made by both services to attempt endoscopic retrieval with the transition to exploratory laparotomy if endoscopy failed. An adult gastroscope was advanced to the distal ileum where the intragastric balloon was identified. There was significant ulceration of ileal mucosa at the site of the intragastric balloon concerning for ischemia. Using an OTSC Twin Grasper the intragastric balloon was punctured and the balloon was further decompressed. The intragastric balloon was then grasped using both arms of the OTSC Twin grasper and was carefully removed through the distal ileum and colon without any complications. The patient tolerated the procedure well and was discharged the following day.
Discussion: Though rare, dislodgement and migration of intragastric balloons can cause serious complications including bowel obstruction. Surgery is often the first-line treatment in patients who are unstable or present with an acute abdomen. Our case illustrates that prompt recognition of intragastric balloon migration causing obstruction can be treated safely with endoscopy if diagnosed early. This can prevent hospital length of stay and morbidity in patients who would otherwise undergo exploratory laparotomy.
Disclosures:
Mena Saad, DO1, Danyal O. Imam, MBBS1, Jun Song, MD2, Harold J. Duarte, MD3, Emily Lin, MD2, Gunnar Wolfe, MD1, Jee Hoon Song, MD2, Christopher Bent, MD1, Wichit Srikureja, MD1, David X. Liu, MD1, John Agapian, MD1, Steve Serrao, MD1. P5100 - Where Did The Balloon Go? A Case of Small Bowel Obstruction Caused by a Displaced Intragastric Balloon, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Riverside University Health System, Moreno Valley, CA; 2Loma Linda University Medical Center, Loma Linda, CA; 3Loma Linda University Health, Loma Linda, CA
Introduction: With the increasing prevalence of obesity in the United States, the intragastric balloon is a minimally invasive option that works by promoting the feeling of satiation. Intestinal obstruction with migration of the balloon remains a rare but serious complication of intragastric balloon. The risk is increased with prolonged use of intragastric balloons due to the risk of balloon deflation and migration throughout the small and large bowel. We present a case of a small bowel obstruction secondary to a migrated intragastric balloon that was managed endoscopically.
Case Description/Methods: The patient is a 43-year-old male with a past medical history significant for an intragastric balloon placed 2 years ago who presents with epigastric abdominal pain, nausea, and vomiting for 3 days prior to admission. On arrival, he was tachycardic but vital signs were otherwise normal. Laboratory findings were significant for lactate of 3.32 and white blood cell count of 7.2. CT of the abdomen and pelvis showed dilated loops of small bowel with air-fluid levels, mild sigmoid diverticulosis, and an impacted intragastric balloon in the distal ileum. Gastroenterology and Surgery were consulted for the removal of the impacted intragastric balloon. A joint decision was made by both services to attempt endoscopic retrieval with the transition to exploratory laparotomy if endoscopy failed. An adult gastroscope was advanced to the distal ileum where the intragastric balloon was identified. There was significant ulceration of ileal mucosa at the site of the intragastric balloon concerning for ischemia. Using an OTSC Twin Grasper the intragastric balloon was punctured and the balloon was further decompressed. The intragastric balloon was then grasped using both arms of the OTSC Twin grasper and was carefully removed through the distal ileum and colon without any complications. The patient tolerated the procedure well and was discharged the following day.
Discussion: Though rare, dislodgement and migration of intragastric balloons can cause serious complications including bowel obstruction. Surgery is often the first-line treatment in patients who are unstable or present with an acute abdomen. Our case illustrates that prompt recognition of intragastric balloon migration causing obstruction can be treated safely with endoscopy if diagnosed early. This can prevent hospital length of stay and morbidity in patients who would otherwise undergo exploratory laparotomy.
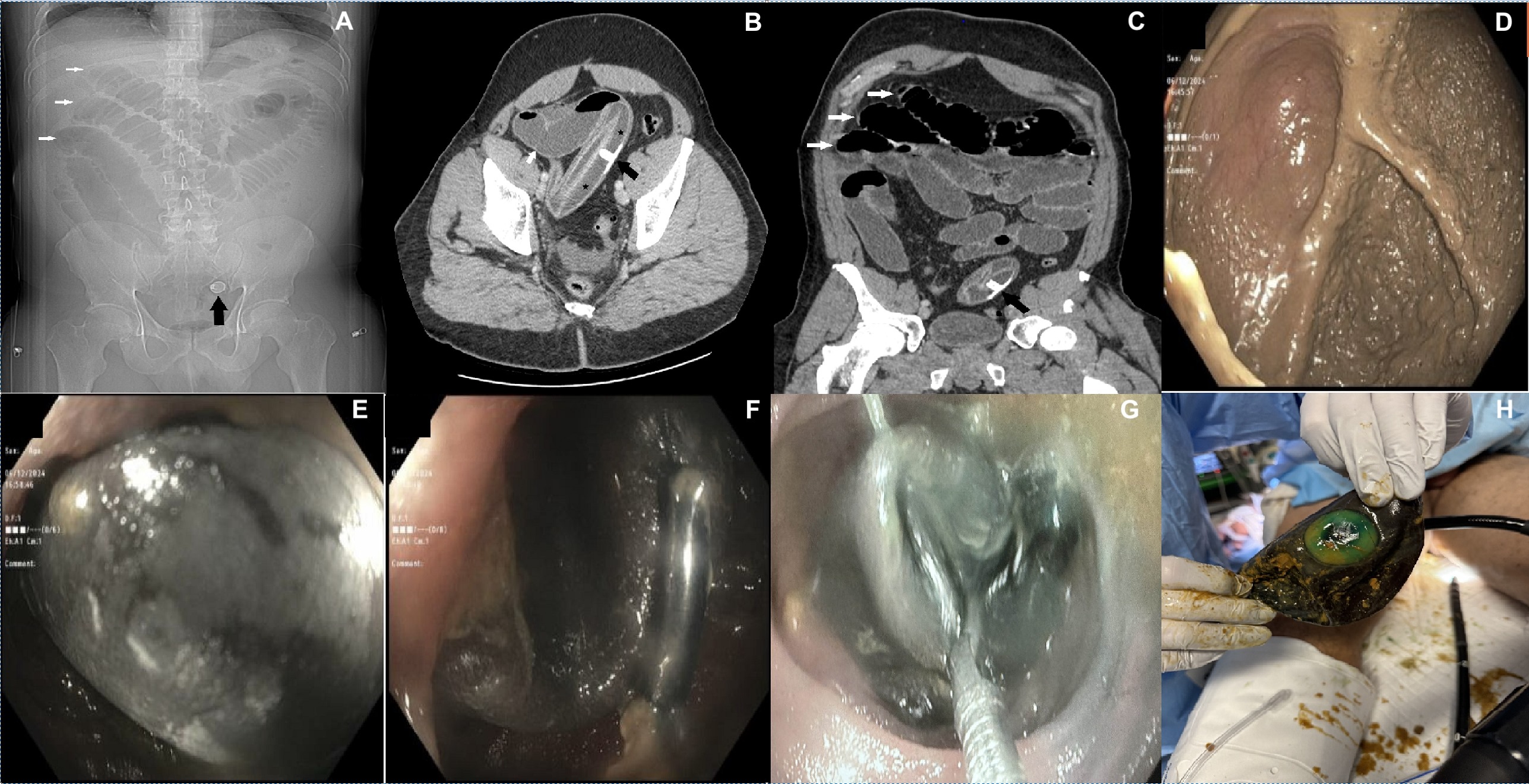
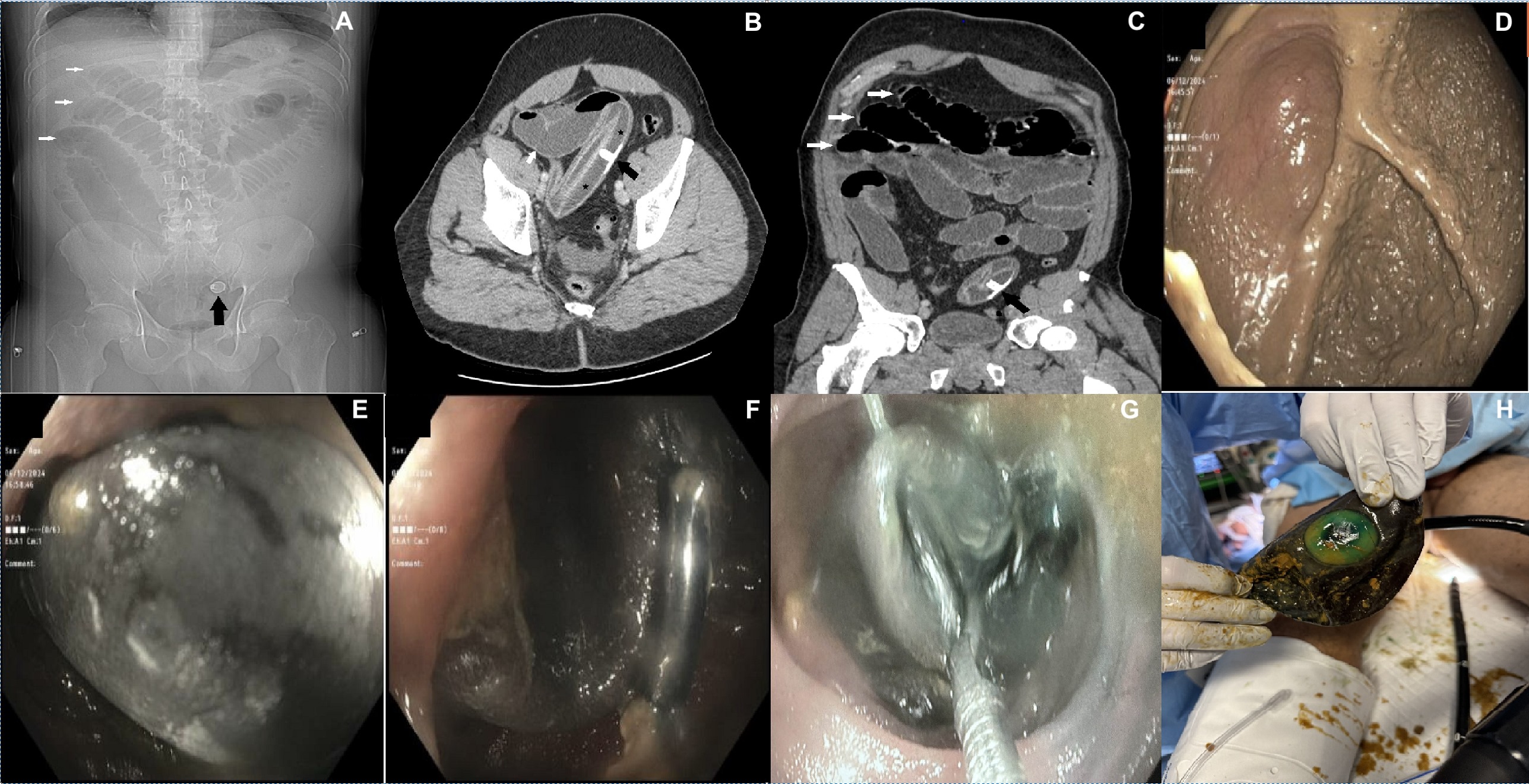
Figure: Figure A: CT scanogram/scout image: black arrow pointing at the intragastric balloon hyperdense port in the distal small bowel, white arrows at dilated obstructed small bowel.
Figure B: CT oblique axial image with IV contrast: black arrow points at the intragastric balloon port in distal small bowel, black stars in the incompletely distended lumen of the balloon, white arrow pointing at distended obstructed small bowel loop.
Figure C: CT oblique coronal image with iv contrast: black arrow points at the intragastric balloon port in distal small bowel, white arrow pointing at distended obstructed small bowel loop.
Figure D: Adult colonoscope advanced to the cecum.
Figure E&F: Intragastric balloon in the distal ileum.
Figure G: Intragastric balloon in the distal ileum grasped with OTSC twin graspers.
Figure H: Deflated intragastric balloon status-post endoscopic removal.
Figure B: CT oblique axial image with IV contrast: black arrow points at the intragastric balloon port in distal small bowel, black stars in the incompletely distended lumen of the balloon, white arrow pointing at distended obstructed small bowel loop.
Figure C: CT oblique coronal image with iv contrast: black arrow points at the intragastric balloon port in distal small bowel, white arrow pointing at distended obstructed small bowel loop.
Figure D: Adult colonoscope advanced to the cecum.
Figure E&F: Intragastric balloon in the distal ileum.
Figure G: Intragastric balloon in the distal ileum grasped with OTSC twin graspers.
Figure H: Deflated intragastric balloon status-post endoscopic removal.
Disclosures:
Mena Saad indicated no relevant financial relationships.
Danyal Imam indicated no relevant financial relationships.
Jun Song indicated no relevant financial relationships.
Harold Duarte indicated no relevant financial relationships.
Emily Lin indicated no relevant financial relationships.
Gunnar Wolfe indicated no relevant financial relationships.
Jee Hoon Song indicated no relevant financial relationships.
Christopher Bent indicated no relevant financial relationships.
Wichit Srikureja indicated no relevant financial relationships.
David Liu indicated no relevant financial relationships.
John Agapian indicated no relevant financial relationships.
Steve Serrao: Provation Medical – Advisory Committee/Board Member.
Mena Saad, DO1, Danyal O. Imam, MBBS1, Jun Song, MD2, Harold J. Duarte, MD3, Emily Lin, MD2, Gunnar Wolfe, MD1, Jee Hoon Song, MD2, Christopher Bent, MD1, Wichit Srikureja, MD1, David X. Liu, MD1, John Agapian, MD1, Steve Serrao, MD1. P5100 - Where Did The Balloon Go? A Case of Small Bowel Obstruction Caused by a Displaced Intragastric Balloon, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

