Tuesday Poster Session
Category: Stomach
P5104 - A Rare Case of Collagenous Gastritis in Patient Presenting With Gastric Perforation
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Haarika Korlipara, MD
New York-Presbyterian / Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Haarika Korlipara, MD1, Emily Smith, MD2, Russell Weg, MD3
1New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian/Weill Cornell, New York, NY; 3Weill Cornell Medicine, New York, NY
Introduction: Collagenous gastritis (CG) is a rare inflammatory condition defined by subepithelial deposition of collagen bands ≥ 10 µm in the lamina propria. Clinical presentation can be heterogeneous and includes abdominal pain, iron deficiency anemia, and diarrhea. Here, we present an atypical case of a young adult with spontaneous gastric perforation in the setting of CG.
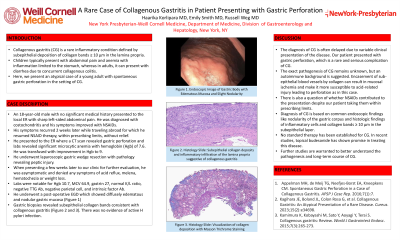
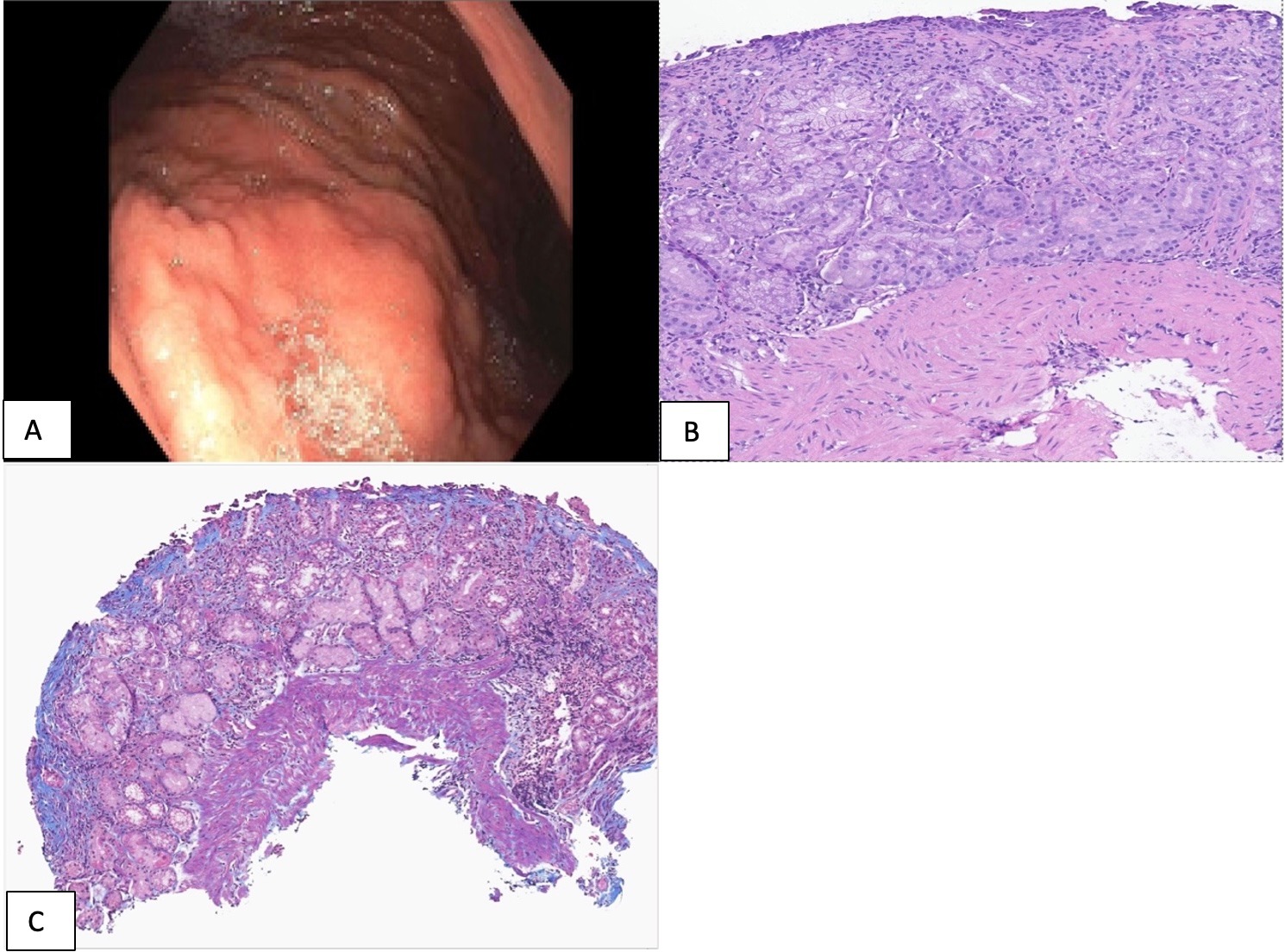
Case Description/Methods: An 18-year-old man presented to the local ER with sharp left-sided abdominal pain. He was diagnosed with costochondritis and improved with NSAIDs. His symptoms recurred 2 weeks later while traveling abroad for which he resumed NSAID therapy, within prescribing limits, without relief. He presented to the ER where CT scan revealed gastric perforation and labs revealed anemia with hemoglobin (Hgb) of 7.6. He denies history of overt GI bleeding. He underwent laparoscopic gastric wedge resection with pathology revealing peptic injury. He presented later to our clinic for further evaluation. He was without any symptoms and labs were notable for Hgb 10.7, MCV 64.9, gastrin 27, normal K/L ratio, negative TTG Ab, negative parietal cell and intrinsic factor Ab. He underwent a post-operative EGD which showed diffusely edematous and nodular gastric mucosa. Gastric biopsies revealed subepithelial collagen bands consistent with CG. There was no evidence of active H pylori infection.
Discussion: The diagnosis of CG is often delayed due to the variable clinical presentation of the disease. Our patient presented with gastric perforation, which is a rare and serious complication of CG. The exact pathogenesis of CG remains unknown, but an autoimmune background is suggested. Encasement of sub-epithelial blood vessels by collagen can result in mucosal ischemia and make it more susceptible to acid-related injury leading to perforation as in the case above. There is also a question of whether NSAIDs contributed to the presentation despite our patient taking them within prescribing limits. Diagnosis of CG is based on common endoscopic findings like nodularity of the gastric corpus and histologic findings of inflammatory cells and collagen bands ≥ 10 µm in the subepithelial layer. No standard therapy has been established for CG and PPI, H2 receptor antagonists, and iron supplementation have been tried with limited success. In recent studies, topical budesonide has shown promise in treating this disease. Further studies are warranted to better understand the pathogenesis and long-term course of CG.
Disclosures:
Haarika Korlipara, MD1, Emily Smith, MD2, Russell Weg, MD3. P5104 - A Rare Case of Collagenous Gastritis in Patient Presenting With Gastric Perforation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian/Weill Cornell, New York, NY; 3Weill Cornell Medicine, New York, NY
Introduction: Collagenous gastritis (CG) is a rare inflammatory condition defined by subepithelial deposition of collagen bands ≥ 10 µm in the lamina propria. Clinical presentation can be heterogeneous and includes abdominal pain, iron deficiency anemia, and diarrhea. Here, we present an atypical case of a young adult with spontaneous gastric perforation in the setting of CG.
Case Description/Methods: An 18-year-old man presented to the local ER with sharp left-sided abdominal pain. He was diagnosed with costochondritis and improved with NSAIDs. His symptoms recurred 2 weeks later while traveling abroad for which he resumed NSAID therapy, within prescribing limits, without relief. He presented to the ER where CT scan revealed gastric perforation and labs revealed anemia with hemoglobin (Hgb) of 7.6. He denies history of overt GI bleeding. He underwent laparoscopic gastric wedge resection with pathology revealing peptic injury. He presented later to our clinic for further evaluation. He was without any symptoms and labs were notable for Hgb 10.7, MCV 64.9, gastrin 27, normal K/L ratio, negative TTG Ab, negative parietal cell and intrinsic factor Ab. He underwent a post-operative EGD which showed diffusely edematous and nodular gastric mucosa. Gastric biopsies revealed subepithelial collagen bands consistent with CG. There was no evidence of active H pylori infection.
Discussion: The diagnosis of CG is often delayed due to the variable clinical presentation of the disease. Our patient presented with gastric perforation, which is a rare and serious complication of CG. The exact pathogenesis of CG remains unknown, but an autoimmune background is suggested. Encasement of sub-epithelial blood vessels by collagen can result in mucosal ischemia and make it more susceptible to acid-related injury leading to perforation as in the case above. There is also a question of whether NSAIDs contributed to the presentation despite our patient taking them within prescribing limits. Diagnosis of CG is based on common endoscopic findings like nodularity of the gastric corpus and histologic findings of inflammatory cells and collagen bands ≥ 10 µm in the subepithelial layer. No standard therapy has been established for CG and PPI, H2 receptor antagonists, and iron supplementation have been tried with limited success. In recent studies, topical budesonide has shown promise in treating this disease. Further studies are warranted to better understand the pathogenesis and long-term course of CG.
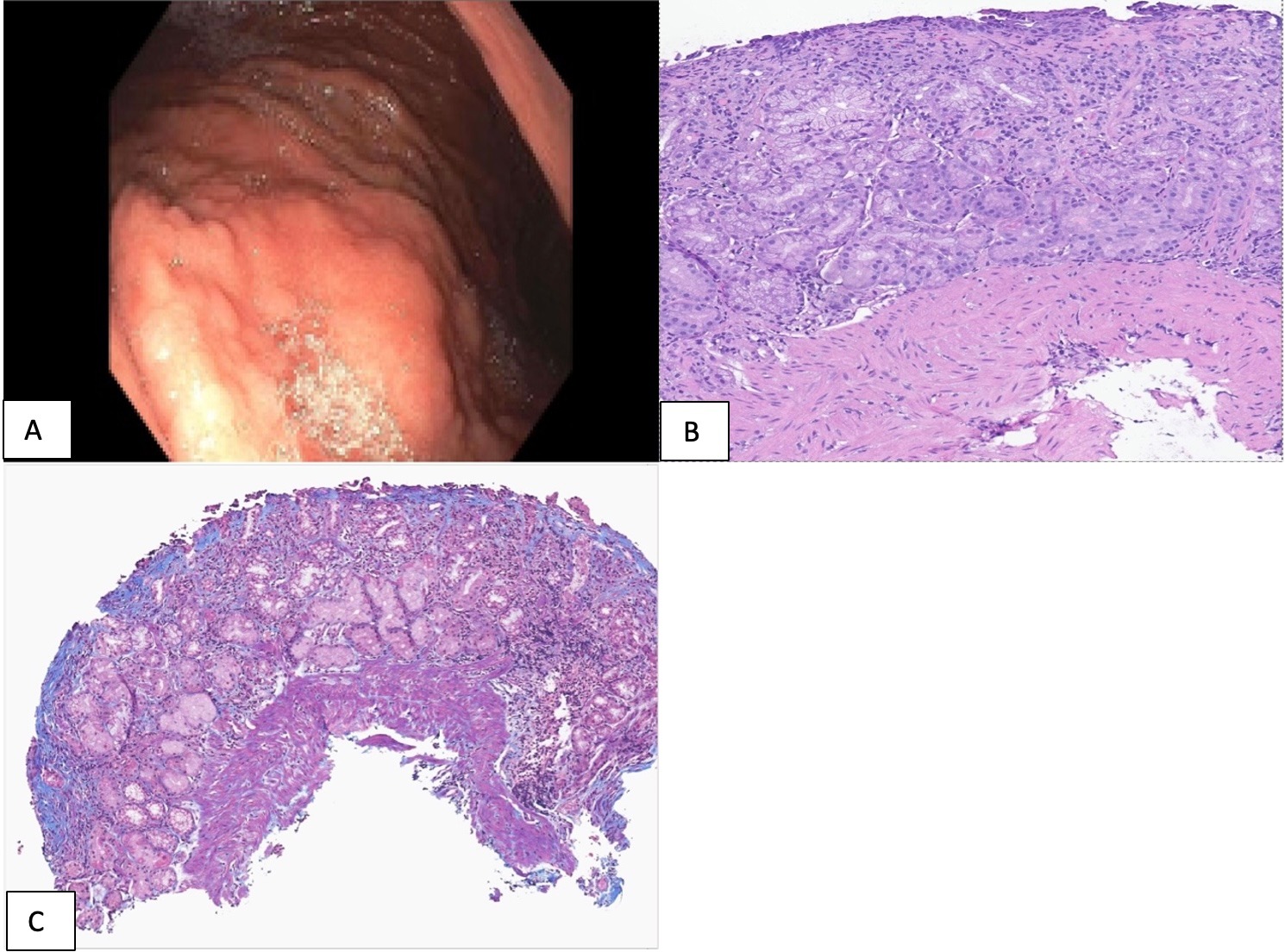
Figure: A. Endoscopic Image of Gastric Body with Edematous Mucosa and Slight Nodularity
B. Histology slide: Subepithelial collagen deposits and inflammatory infiltration of the lamina propria suggestive of Collagenous Gastritis
C. Histology slide: Visualization of collagen deposition with Masson Trichrome staining
B. Histology slide: Subepithelial collagen deposits and inflammatory infiltration of the lamina propria suggestive of Collagenous Gastritis
C. Histology slide: Visualization of collagen deposition with Masson Trichrome staining
Disclosures:
Haarika Korlipara indicated no relevant financial relationships.
Emily Smith indicated no relevant financial relationships.
Russell Weg indicated no relevant financial relationships.
Haarika Korlipara, MD1, Emily Smith, MD2, Russell Weg, MD3. P5104 - A Rare Case of Collagenous Gastritis in Patient Presenting With Gastric Perforation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
