Tuesday Poster Session
Category: Stomach
P5108 - Distinguishing Primary Gastric Leiomyosarcoma from a Gastrointestinal Stromal Tumour: A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AR
Amrik SC Randhawa, MD
University of Saskatchewan
Saskatoon, SK, Canada
Presenting Author(s)
Amrik SC. Randhawa, MD, Mina Niazi, MD, Branawan Gowrishankar, MD
University of Saskatchewan, Saskatoon, SK, Canada
Introduction: Primary gastric leiomyosarcoma (LMS) comprises 1% of stomach tumors. Historically, gastric LMS were misdiagnosed as gastrointestinal stromal tumors (GIST), but immunohistochemistry allows differentiation. GISTs are positive for CD117, DOG1 and PDGFRA mutation, whereas gastric LMS tumors are typically positive for smooth muscle actin (SMA) and desmin. This case highlights the importance of distinguishing a gastric LMS from a GIST in a patient with metastatic disease.
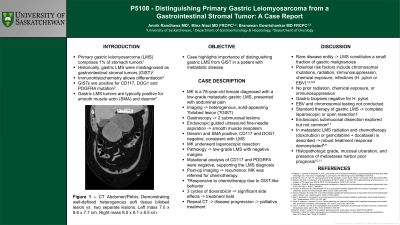
Case Description/Methods: MK is a 78-year-old female diagnosed with a low-grade metastatic gastric LMS, initially presenting with abdominal pain. Imaging visualized a large heterogenous, solid-appearing possibly bilobed lesion suspected to be a GIST. Gastroscopy identified two submucosal lesions. Endoscopic guided ultrasound fine-needle aspiration demonstrated a smooth muscle neoplasm. It was desmin and SMA positive, while CD117 and DOG1 negative, consistent with LMS. MK underwent laparoscopic resection. Pathology was consistent with low-grade LMS with negative margins. Furthermore, mutational analysis of CD117 and PDGRFA were negative, supporting the LMS diagnosis.
Post-operative follow-up imaging demonstrated recurrence and MK was referred for chemotherapy. The LMS was suspected to be responsive to chemotherapy due to its GIST-like behaviour. She received three cycles of doxorubicin but unfortunately developed significant side effects and therefore treatment was held. Repeat CT demonstrated disease progression and the decision was made to pursue palliative treatment.
Discussion: Our case report highlights a rare disease entity, as LMS constitutes a small fraction of gastric malignancies. Potential risk factors include chromosomal mutations, radiation, immunosuppression, chemical exposure and infections such as Helicobacter pylori or Epstein-Barr virus. MK had no prior radiation, chemical exposure, or immunosuppression. Gastric biopsies were negative for Helicobacter pylori infection. However, Epstein-Barr virus and chromosomal testing were not conducted. Standard therapy of gastric LMS involves complete laparoscopic or open resection. Endoscopic submucosal dissection has been explored but is not common. In metastatic LMS radiation and chemotherapy, with doxorubicin or a regimen of gemcitabine with docetaxel, is described. Yet no robust treatment response is demonstrated with available agents. Histopathologic grade, mucosal ulceration, and presence of metastases harbor poor prognosis.
Disclosures:
Amrik SC. Randhawa, MD, Mina Niazi, MD, Branawan Gowrishankar, MD. P5108 - Distinguishing Primary Gastric Leiomyosarcoma from a Gastrointestinal Stromal Tumour: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Saskatchewan, Saskatoon, SK, Canada
Introduction: Primary gastric leiomyosarcoma (LMS) comprises 1% of stomach tumors. Historically, gastric LMS were misdiagnosed as gastrointestinal stromal tumors (GIST), but immunohistochemistry allows differentiation. GISTs are positive for CD117, DOG1 and PDGFRA mutation, whereas gastric LMS tumors are typically positive for smooth muscle actin (SMA) and desmin. This case highlights the importance of distinguishing a gastric LMS from a GIST in a patient with metastatic disease.
Case Description/Methods: MK is a 78-year-old female diagnosed with a low-grade metastatic gastric LMS, initially presenting with abdominal pain. Imaging visualized a large heterogenous, solid-appearing possibly bilobed lesion suspected to be a GIST. Gastroscopy identified two submucosal lesions. Endoscopic guided ultrasound fine-needle aspiration demonstrated a smooth muscle neoplasm. It was desmin and SMA positive, while CD117 and DOG1 negative, consistent with LMS. MK underwent laparoscopic resection. Pathology was consistent with low-grade LMS with negative margins. Furthermore, mutational analysis of CD117 and PDGRFA were negative, supporting the LMS diagnosis.
Post-operative follow-up imaging demonstrated recurrence and MK was referred for chemotherapy. The LMS was suspected to be responsive to chemotherapy due to its GIST-like behaviour. She received three cycles of doxorubicin but unfortunately developed significant side effects and therefore treatment was held. Repeat CT demonstrated disease progression and the decision was made to pursue palliative treatment.
Discussion: Our case report highlights a rare disease entity, as LMS constitutes a small fraction of gastric malignancies. Potential risk factors include chromosomal mutations, radiation, immunosuppression, chemical exposure and infections such as Helicobacter pylori or Epstein-Barr virus. MK had no prior radiation, chemical exposure, or immunosuppression. Gastric biopsies were negative for Helicobacter pylori infection. However, Epstein-Barr virus and chromosomal testing were not conducted. Standard therapy of gastric LMS involves complete laparoscopic or open resection. Endoscopic submucosal dissection has been explored but is not common. In metastatic LMS radiation and chemotherapy, with doxorubicin or a regimen of gemcitabine with docetaxel, is described. Yet no robust treatment response is demonstrated with available agents. Histopathologic grade, mucosal ulceration, and presence of metastases harbor poor prognosis.
Disclosures:
Amrik Randhawa indicated no relevant financial relationships.
Mina Niazi indicated no relevant financial relationships.
Branawan Gowrishankar indicated no relevant financial relationships.
Amrik SC. Randhawa, MD, Mina Niazi, MD, Branawan Gowrishankar, MD. P5108 - Distinguishing Primary Gastric Leiomyosarcoma from a Gastrointestinal Stromal Tumour: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
