Tuesday Poster Session
Category: Stomach
P5118 - Gastric Neuroendocrine Tumor Induced by Long-Term PPI Use
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sapana R. Gupta, MD
Brown University / Rhode Island Hospital
Providence, RI
Presenting Author(s)
Sapana R. Gupta, MD1, Lindsey Channen, MD2, Fadlallah Habr, MD3
1Brown University / Rhode Island Hospital, Providence, RI; 2Brown Medicine/Lifespan, Providence, RI; 3Rhode Island Hospital, Providence, RI
Introduction: The incidence and prevalence of neuroendocrine tumors (NETs) has been increasing, especially gastrointestinal NETs. The incidence of pathogenic influences such as Zollinger-Ellison Syndrome, multiple endocrine neoplasia type 1, and chronic atrophic gastritis have remained largely unchanged. Thus, the etiology of this trend is likely multifactorial and affected by biologic and environmental factors. Notably, there has been an parallel increase use of prolonged PPIs. This case describes a gentleman with a 20-year history of PPI use with a gastric neuroendocrine tumor.
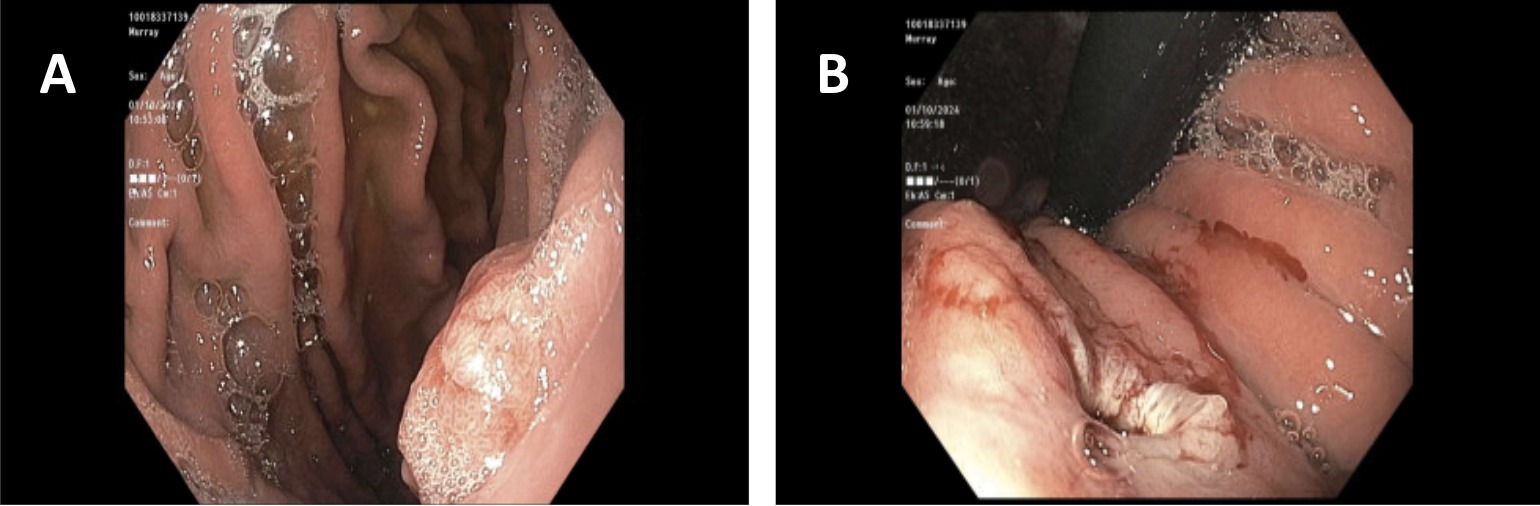
Case Description/Methods: A 50-year-old male with a past medical history of hypertension and diabetes mellitus presented to the outpatient setting for epigastric pain. He was taking esomeprazole daily for twenty years. Otherwise, he denied any unintentional weight loss, dysphagia, or melenic stool. Family history was non-contributory. Initial EGD revealed a normal appearance of the gastroesophageal junction without esophagitis and a 10mm, sessile polyp without evidence of atrophic gastritis. Colonoscopy revealed two polyps, which were resected and retrieved. On pathology, the sessile gastric fundus polyp was consistent with a well-differentiated neuroendocrine tumor. Ki-67 estimated 6.5% and one mitotic figure per ten high-power field consistent with a grade 2 tumor. Gastrin level was 47 after esomeprazole was held for two days. However, after oncology referral, it was recommended a gastrin level was obtained while the patient was on his PPI to mimic his natural state. Repeat gastrin level was elevated at 145. Endoscopic mucosal resection revealed a 0.9cm tumor in the fundus extending to the submucosa with pathologic stage pT1, pNx. PET-CT with Dotatate for staging revealed a 3 mm anterior right upper lobe lung nodule and a 5 mm right middle lobe lung nodule, without focal radiotracer uptake. There was mild, diffuse uptake within the gastric fundus and body which may be physiologic or infectious/inflammatory. No Dotatate tracer demonstrating lymphadenopathy within the abdomen or pelvis was visualized.
Discussion: Several cases have been reported associating extended PPI use and gastric NETs, but only one other case reported PPI duration of at least two decades. The likely mechanism is hypergastrinemia leading to enterochromaffin-like cell hyperplasia. However, only a few patients transition from dysplasia to neoplasia, indicating biologic and environmental influences are likely involved.
Disclosures:
Sapana R. Gupta, MD1, Lindsey Channen, MD2, Fadlallah Habr, MD3. P5118 - Gastric Neuroendocrine Tumor Induced by Long-Term PPI Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brown University / Rhode Island Hospital, Providence, RI; 2Brown Medicine/Lifespan, Providence, RI; 3Rhode Island Hospital, Providence, RI
Introduction: The incidence and prevalence of neuroendocrine tumors (NETs) has been increasing, especially gastrointestinal NETs. The incidence of pathogenic influences such as Zollinger-Ellison Syndrome, multiple endocrine neoplasia type 1, and chronic atrophic gastritis have remained largely unchanged. Thus, the etiology of this trend is likely multifactorial and affected by biologic and environmental factors. Notably, there has been an parallel increase use of prolonged PPIs. This case describes a gentleman with a 20-year history of PPI use with a gastric neuroendocrine tumor.
Case Description/Methods: A 50-year-old male with a past medical history of hypertension and diabetes mellitus presented to the outpatient setting for epigastric pain. He was taking esomeprazole daily for twenty years. Otherwise, he denied any unintentional weight loss, dysphagia, or melenic stool. Family history was non-contributory. Initial EGD revealed a normal appearance of the gastroesophageal junction without esophagitis and a 10mm, sessile polyp without evidence of atrophic gastritis. Colonoscopy revealed two polyps, which were resected and retrieved. On pathology, the sessile gastric fundus polyp was consistent with a well-differentiated neuroendocrine tumor. Ki-67 estimated 6.5% and one mitotic figure per ten high-power field consistent with a grade 2 tumor. Gastrin level was 47 after esomeprazole was held for two days. However, after oncology referral, it was recommended a gastrin level was obtained while the patient was on his PPI to mimic his natural state. Repeat gastrin level was elevated at 145. Endoscopic mucosal resection revealed a 0.9cm tumor in the fundus extending to the submucosa with pathologic stage pT1, pNx. PET-CT with Dotatate for staging revealed a 3 mm anterior right upper lobe lung nodule and a 5 mm right middle lobe lung nodule, without focal radiotracer uptake. There was mild, diffuse uptake within the gastric fundus and body which may be physiologic or infectious/inflammatory. No Dotatate tracer demonstrating lymphadenopathy within the abdomen or pelvis was visualized.
Discussion: Several cases have been reported associating extended PPI use and gastric NETs, but only one other case reported PPI duration of at least two decades. The likely mechanism is hypergastrinemia leading to enterochromaffin-like cell hyperplasia. However, only a few patients transition from dysplasia to neoplasia, indicating biologic and environmental influences are likely involved.
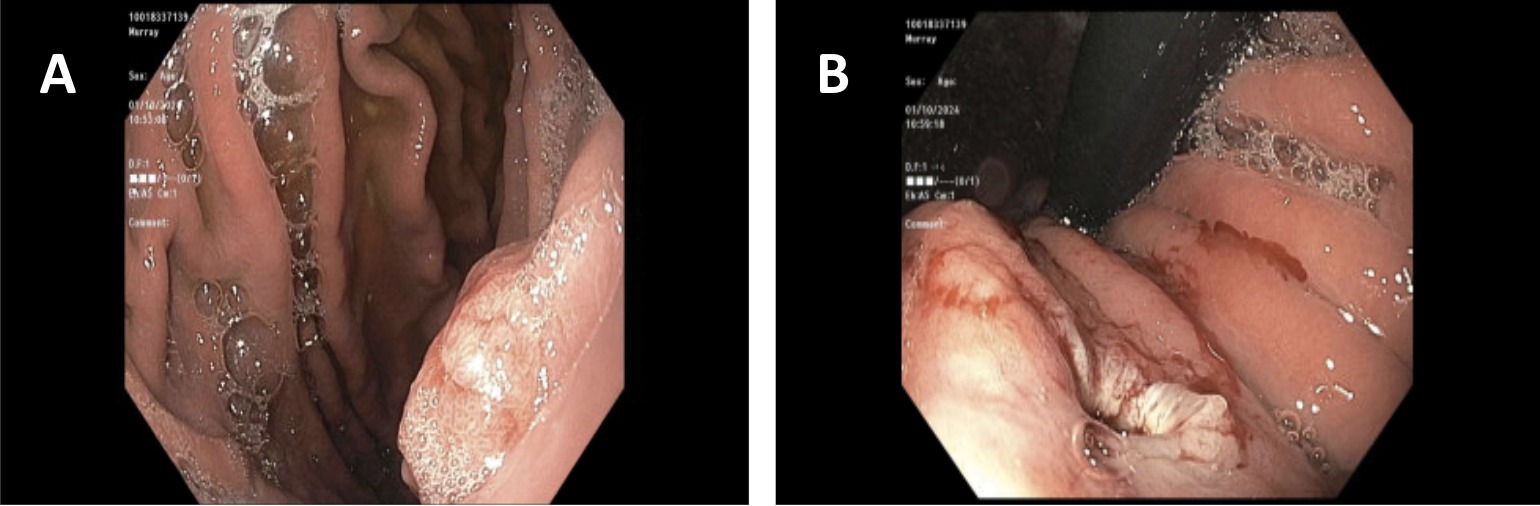
Figure: Figure 1: A) Gastric fundus neuroendocrine tumor, B) Endoscopic mucosal resection of neuroendocrine tumor
Disclosures:
Sapana Gupta indicated no relevant financial relationships.
Lindsey Channen indicated no relevant financial relationships.
Fadlallah Habr indicated no relevant financial relationships.
Sapana R. Gupta, MD1, Lindsey Channen, MD2, Fadlallah Habr, MD3. P5118 - Gastric Neuroendocrine Tumor Induced by Long-Term PPI Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
