Tuesday Poster Session
Category: Stomach
P5125 - Gastric Perforation as a Manifestation of Eosinophilic Gastroenteritis: An Exceptionally Rare Occurrence
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Muhammad Ali Butt, MD
Allegheny General Hospital
Pittsburgh, PA
Presenting Author(s)
Muhammad Ali Butt, MD1, Taimur S. Muzammil, MD1, Himsikhar Khataniar, MD1, Rahul Karna, MD2, Usman Tariq, MD3, Rachel Toney, MD3
1Allegheny General Hospital, Pittsburgh, PA; 2University of Minnesota Medical Center, Minneapolis, MN; 3Allegheny Center for Digestive Health, Pittsburgh, PA
Introduction: Eosinophilic gastroenteritis (EG) is a challenging diagnosis due to its chronic, recurrent nature and symptom overlap with various gastrointestinal (GI) disorders which often leads to underdiagnosis and delays in appropriate treatment. Here, we present a rare case of gastric perforation associated with EG, highlighting the need for increased vigilance and timely diagnosis in managing this condition.
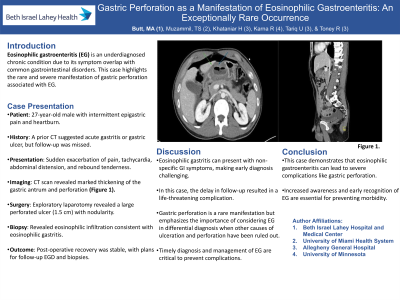
Case Description/Methods: A 27-year-old male with a medical history of intermittent epigastric pain and heartburn presented to the Emergency Department with a sudden exacerbation of long-standing epigastric pain. A prior Computed Tomography (CT) scan had suggested acute gastritis or gastric ulcer disease, with a recommendation of gastroenterology follow-up that the patient did not pursue. On presentation, the patient was tachycardic and normotensive on room air. His examination was remarkable for signs of abdominal distension with rebound tenderness. Initial Laboratory data showed elevated white blood cell count and otherwise unremarkable complete blood count, Basic metabolic panel and lipase levels. Subsequently a CT scan was completed which showed marked thickening of the gastric antrum with perforation seen along its anterior superior wall with moderate volume of pneumoperitoneum and small volume abdominopelvic free fluid (Figure 1). The patient underwent an emergent exploratory laparotomy. Intraoperatively a large, perforated ulcer (1.5 cm) with significant surrounding induration and nodularity was noted on the anterior wall of the stomach requiring omental repair. Intraoperative Esophagogastroduodenoscopy (EGD) was performed and 2 biopsies of the mucosa surrounding the ulcer were taken. The biopsy results showed fragments of antral type gastric mucosa, foveolar epithelium with granulation tissue, and focally prominent eosinophils (consistent with ulcer and eosinophilic gastritis). Patient remained stable post-operatively, and subsequently discharged home with plans for repeat EGD in 8 weeks to assess for ulcer healing and repeat biopsies.
Discussion: The patient's chronic symptoms, along with a history of neglected follow-up, contributed to the delay in identifying EG. This case reports gastric perforation as an extremely rare manifestation of EG and also underscores the significance of early diagnosis and prompt treatment for EG, as if left untreated can result in severe complications leading to increased morbidity in patients.

Disclosures:
Muhammad Ali Butt, MD1, Taimur S. Muzammil, MD1, Himsikhar Khataniar, MD1, Rahul Karna, MD2, Usman Tariq, MD3, Rachel Toney, MD3. P5125 - Gastric Perforation as a Manifestation of Eosinophilic Gastroenteritis: An Exceptionally Rare Occurrence, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Allegheny General Hospital, Pittsburgh, PA; 2University of Minnesota Medical Center, Minneapolis, MN; 3Allegheny Center for Digestive Health, Pittsburgh, PA
Introduction: Eosinophilic gastroenteritis (EG) is a challenging diagnosis due to its chronic, recurrent nature and symptom overlap with various gastrointestinal (GI) disorders which often leads to underdiagnosis and delays in appropriate treatment. Here, we present a rare case of gastric perforation associated with EG, highlighting the need for increased vigilance and timely diagnosis in managing this condition.
Case Description/Methods: A 27-year-old male with a medical history of intermittent epigastric pain and heartburn presented to the Emergency Department with a sudden exacerbation of long-standing epigastric pain. A prior Computed Tomography (CT) scan had suggested acute gastritis or gastric ulcer disease, with a recommendation of gastroenterology follow-up that the patient did not pursue. On presentation, the patient was tachycardic and normotensive on room air. His examination was remarkable for signs of abdominal distension with rebound tenderness. Initial Laboratory data showed elevated white blood cell count and otherwise unremarkable complete blood count, Basic metabolic panel and lipase levels. Subsequently a CT scan was completed which showed marked thickening of the gastric antrum with perforation seen along its anterior superior wall with moderate volume of pneumoperitoneum and small volume abdominopelvic free fluid (Figure 1). The patient underwent an emergent exploratory laparotomy. Intraoperatively a large, perforated ulcer (1.5 cm) with significant surrounding induration and nodularity was noted on the anterior wall of the stomach requiring omental repair. Intraoperative Esophagogastroduodenoscopy (EGD) was performed and 2 biopsies of the mucosa surrounding the ulcer were taken. The biopsy results showed fragments of antral type gastric mucosa, foveolar epithelium with granulation tissue, and focally prominent eosinophils (consistent with ulcer and eosinophilic gastritis). Patient remained stable post-operatively, and subsequently discharged home with plans for repeat EGD in 8 weeks to assess for ulcer healing and repeat biopsies.
Discussion: The patient's chronic symptoms, along with a history of neglected follow-up, contributed to the delay in identifying EG. This case reports gastric perforation as an extremely rare manifestation of EG and also underscores the significance of early diagnosis and prompt treatment for EG, as if left untreated can result in severe complications leading to increased morbidity in patients.

Figure: CT scan showing marked thickening of the gastric antrum (Blue Arrow) with perforation seen along its anterior superior wall (Green arrow).
Disclosures:
Muhammad Ali Butt indicated no relevant financial relationships.
Taimur Muzammil indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Usman Tariq indicated no relevant financial relationships.
Rachel Toney indicated no relevant financial relationships.
Muhammad Ali Butt, MD1, Taimur S. Muzammil, MD1, Himsikhar Khataniar, MD1, Rahul Karna, MD2, Usman Tariq, MD3, Rachel Toney, MD3. P5125 - Gastric Perforation as a Manifestation of Eosinophilic Gastroenteritis: An Exceptionally Rare Occurrence, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
