Tuesday Poster Session
Category: Stomach
P5133 - Hidden Hairball Hazard: A Case of Gastric Perforation With Purulent Peritonitis Due to an Insidious Trichobezoar
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Muhammad Usman Javed, MBBS
Services Hospital
Lahore, Punjab, Pakistan
Presenting Author(s)
Award: Presidential Poster Award
Fatima Zafar, MBBS1, Muhammad Usman Javed, MBBS1, Iqra Nawaz, MBBS, BSc2, Muhammad Romail Manan, MBBS, BSc1, Ahmad Zain, MD3, Mahnoor Sultana, MBBS1, Muhammad Imtanan Fazal, MD4
1Services Hospital, Lahore, Punjab, Pakistan; 2Bahawal Victoria Hospital, Bahawalpur, Punjab, Pakistan; 3UChealth Parkview Medical Center, Pueblo, CO; 4Services Institute of Medical Sciences, Lahore, Punjab, Pakistan
Introduction: Trichobezoar, a rare conglomeration of hair within the stomach, is commonly overlooked upon initial presentation resulting in delayed diagnosis, which may lead to severe complications. Additionally, its rare but complicated nature makes it an important differential diagnosis. We aim to highlight the atypical presentation of trichobezoar in a patient, diverging from the typical clinical course observed in such cases.
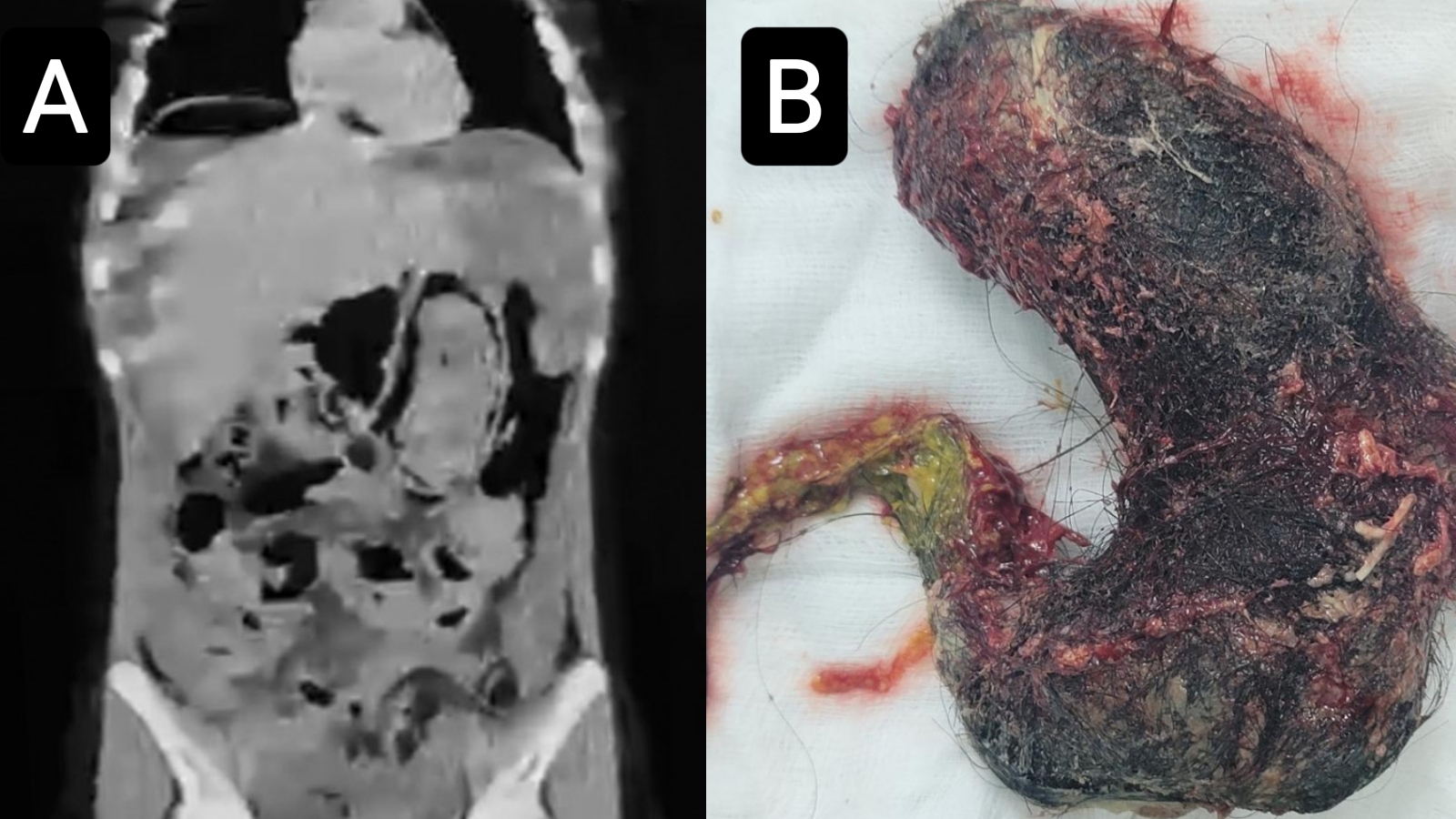
Case Description/Methods: We describe the case of a 16-year-old female with unremarkable past medical history who presented to the emergency room with a 3-day history of worsening abdominal pain with one episode of non-bilious vomiting and anorexia. Upon presentation, she was hypotensive (90 / 60 mm of Hg), tachypnoeic (20 breaths per minute), and tachycardic (105 beats per minute) but afebrile, with a distended abdomen exhibiting signs of generalized peritonitis. An abdominal CT scan obtained following initial resuscitation revealed pneumoperitoneum and a large trichobezoar.
With a diagnosis of perforated acute abdomen, an emergency exploratory laparotomy was performed. Intraoperatively, a gastric perforation measuring 1cm x 1 cm in the anterior wall of the stomach was found and 1 litre of purulent fluid was removed. Anterior gastrotomy was performed midway between lesser and greater curvature of the stomach. A hard trichobezoar, measuring 20 cm x 10 cm moulded into the shape of the stomach with the tail extending beyond the pylorus, was extracted en bloc; and double-layer repair of the gastric wall was performed along with the placement of an omental patch. Her postoperative period was uneventful, and she was discharged on the 6th post-op day with a referral to the psychiatric department.
Discussion: Enteric fever-associated perforation was suspected initially, considering the endemic nature and low socioeconomic background of the patient. However, CT scan imaging was instrumental in finding the cause of the acute abdomen. Exploratory laparotomy surpasses laparoscopic or endoscopic approaches in acute fatal presentation of trichobezoar, allowing successful removal and effective gut repair. Psychiatric factors leading to the disease can go unrecognized leading to recurrence thus psychiatric assessment and close follow-up are imperative.
Disclosures:
Fatima Zafar, MBBS1, Muhammad Usman Javed, MBBS1, Iqra Nawaz, MBBS, BSc2, Muhammad Romail Manan, MBBS, BSc1, Ahmad Zain, MD3, Mahnoor Sultana, MBBS1, Muhammad Imtanan Fazal, MD4. P5133 - Hidden Hairball Hazard: A Case of Gastric Perforation With Purulent Peritonitis Due to an Insidious Trichobezoar, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Fatima Zafar, MBBS1, Muhammad Usman Javed, MBBS1, Iqra Nawaz, MBBS, BSc2, Muhammad Romail Manan, MBBS, BSc1, Ahmad Zain, MD3, Mahnoor Sultana, MBBS1, Muhammad Imtanan Fazal, MD4
1Services Hospital, Lahore, Punjab, Pakistan; 2Bahawal Victoria Hospital, Bahawalpur, Punjab, Pakistan; 3UChealth Parkview Medical Center, Pueblo, CO; 4Services Institute of Medical Sciences, Lahore, Punjab, Pakistan
Introduction: Trichobezoar, a rare conglomeration of hair within the stomach, is commonly overlooked upon initial presentation resulting in delayed diagnosis, which may lead to severe complications. Additionally, its rare but complicated nature makes it an important differential diagnosis. We aim to highlight the atypical presentation of trichobezoar in a patient, diverging from the typical clinical course observed in such cases.
Case Description/Methods: We describe the case of a 16-year-old female with unremarkable past medical history who presented to the emergency room with a 3-day history of worsening abdominal pain with one episode of non-bilious vomiting and anorexia. Upon presentation, she was hypotensive (90 / 60 mm of Hg), tachypnoeic (20 breaths per minute), and tachycardic (105 beats per minute) but afebrile, with a distended abdomen exhibiting signs of generalized peritonitis. An abdominal CT scan obtained following initial resuscitation revealed pneumoperitoneum and a large trichobezoar.
With a diagnosis of perforated acute abdomen, an emergency exploratory laparotomy was performed. Intraoperatively, a gastric perforation measuring 1cm x 1 cm in the anterior wall of the stomach was found and 1 litre of purulent fluid was removed. Anterior gastrotomy was performed midway between lesser and greater curvature of the stomach. A hard trichobezoar, measuring 20 cm x 10 cm moulded into the shape of the stomach with the tail extending beyond the pylorus, was extracted en bloc; and double-layer repair of the gastric wall was performed along with the placement of an omental patch. Her postoperative period was uneventful, and she was discharged on the 6th post-op day with a referral to the psychiatric department.
Discussion: Enteric fever-associated perforation was suspected initially, considering the endemic nature and low socioeconomic background of the patient. However, CT scan imaging was instrumental in finding the cause of the acute abdomen. Exploratory laparotomy surpasses laparoscopic or endoscopic approaches in acute fatal presentation of trichobezoar, allowing successful removal and effective gut repair. Psychiatric factors leading to the disease can go unrecognized leading to recurrence thus psychiatric assessment and close follow-up are imperative.
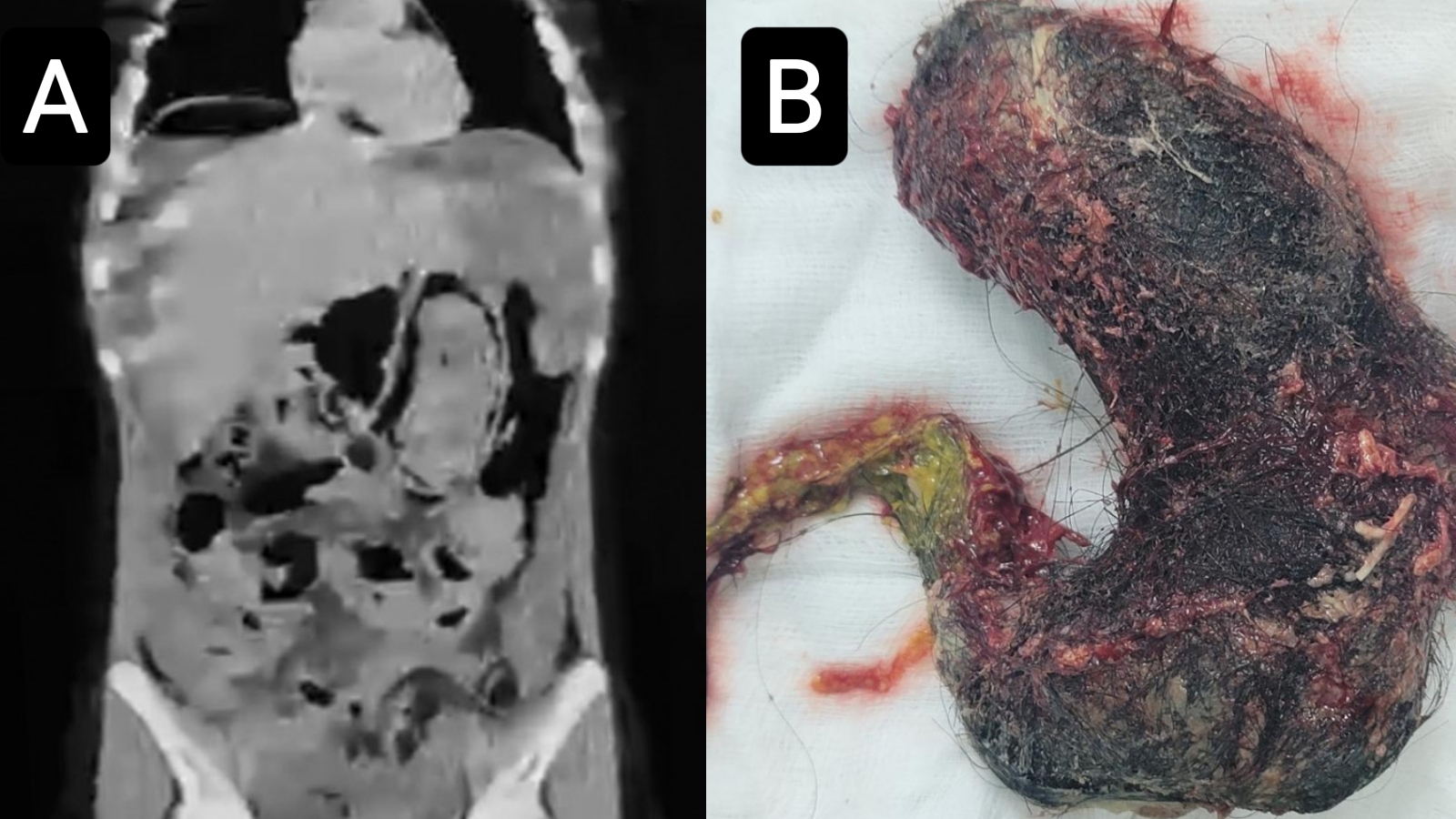
Figure: A. Coronal CT abdomen confirming the presence of gastric bezoar.
B. Surgically removed trichobezoar measuring 20 cm in length and 10 cm width at the widest point.
B. Surgically removed trichobezoar measuring 20 cm in length and 10 cm width at the widest point.
Disclosures:
Fatima Zafar indicated no relevant financial relationships.
Muhammad Usman Javed indicated no relevant financial relationships.
Iqra Nawaz indicated no relevant financial relationships.
Muhammad Romail Manan indicated no relevant financial relationships.
Ahmad Zain indicated no relevant financial relationships.
Mahnoor Sultana indicated no relevant financial relationships.
Muhammad Imtanan Fazal indicated no relevant financial relationships.
Fatima Zafar, MBBS1, Muhammad Usman Javed, MBBS1, Iqra Nawaz, MBBS, BSc2, Muhammad Romail Manan, MBBS, BSc1, Ahmad Zain, MD3, Mahnoor Sultana, MBBS1, Muhammad Imtanan Fazal, MD4. P5133 - Hidden Hairball Hazard: A Case of Gastric Perforation With Purulent Peritonitis Due to an Insidious Trichobezoar, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

