Tuesday Poster Session
Category: Stomach
P5137 - Gastrointestinal Amyloidosis: An Uncommon Cause of GI Bleeding
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Isha Samreen, MBBS, MPH
Hemet Global Medical Center
Murrieta, CA
Presenting Author(s)
Isha Samreen, MBBS, MPH1, Pooja Magavi, MD2, Ashwini Mulgaonkar, MD3, Rohit Khanna, DO4, Behnam Jahromi, MD2
1Hemet Global Medical Center, Murrieta, CA; 2Scripps Clinic, San Diego, CA; 3Scripps Green Hospital, La Jolla, CA; 4Scripps Green Hospital, San Diego, CA
Introduction: Systemic amyloidosis refers to a group of disorders characterized by misfolded protein deposition that can involve various organs. It is commonly associated with chronic inflammatory disorders, hematological malignancy and end-stage renal disease (ESRD). Gastrointestinal (GI) amyloidosis refers to the deposition of such proteins that in turn can interfere with the structure and function of GI organs, predominantly the liver and small bowel. We present a case of amyloidosis with gastric involvement.
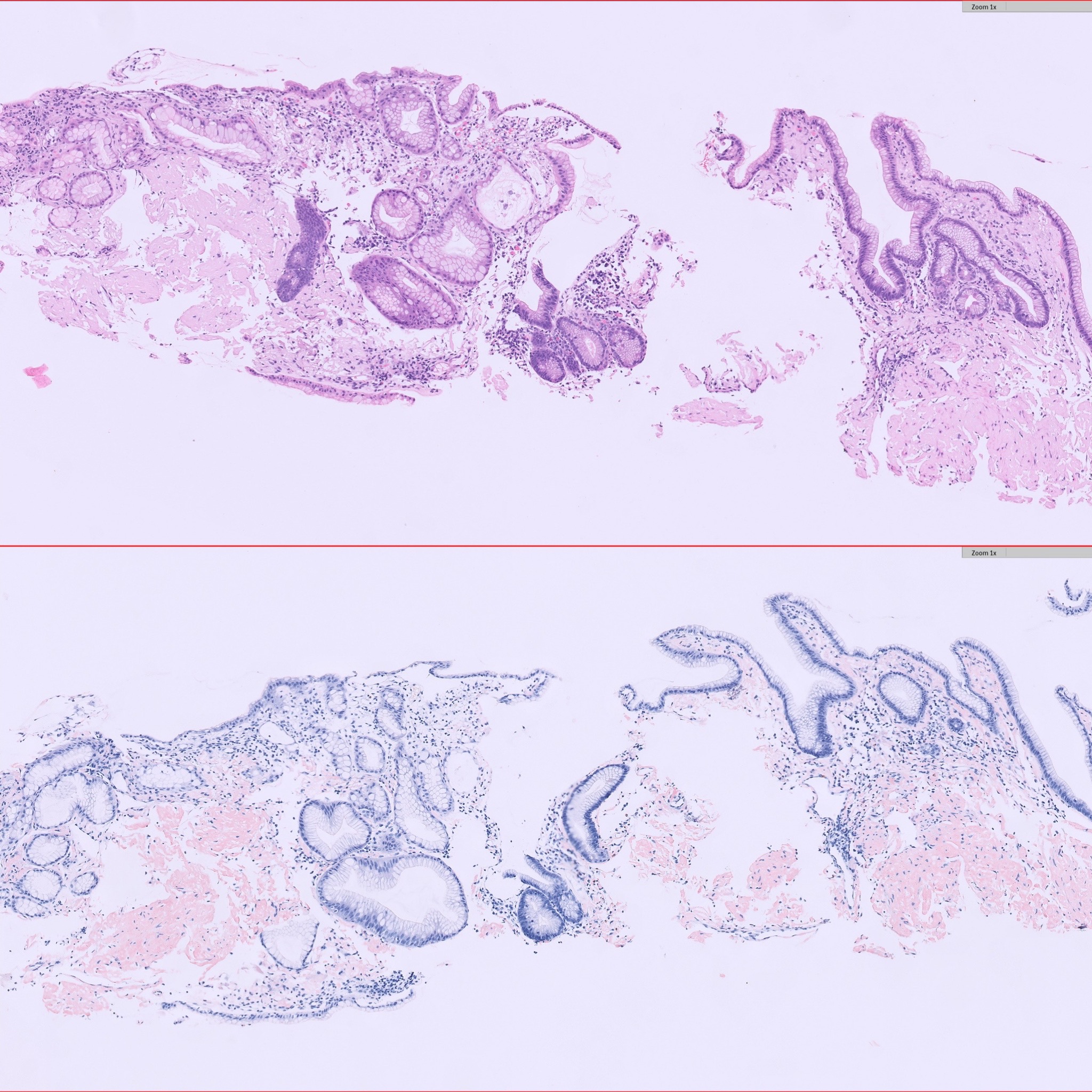
Case Description/Methods: An 80-year-old Caucasian male with history of coronary artery disease, atrial fibrillation, Roux-en-Y gastric bypass (RYGB), ESRD on peritoneal dialysis and traumatic subdural hematoma initially presented to the emergency room after a fall with atrial fibrillation with rapid ventricular response, for which he was started on a heparin drip. He subsequently developed abdominal pain and melena, with a drop in hemoglobin from 8.5 to 7.9. mg/dL. Upper endoscopy showed evidence of bypass anatomy without active bleeding. However, the gastric mucosa was noted to be edematous with areas of friability and oozing on contact, and multiple cold forceps biopsies were obtained. Histological examination revealed abundant amyloid deposition in the lamina propria and blood vessels, confirmed with Congo red staining (Figure 1). The patient was ultimately diagnosed with AL amyloidosis with gastric involvement. He was evaluated by oncology, started on bortezemib and dexamethasone, and referred to cardiology in the setting of atrial fibrillation and elevated NT-proBNP for further cardiac evaluation. He was also presumed to have neurologic involvement manifesting as peripheral neuropathy and renal involvement worsening his ESRD.
Discussion: Gastrointestinal amyloidosis can present with nonspecific symptoms, including fatigue, abdominal pain and weight loss, mimicking other GI disorders. A high degree of clinical suspicion is necessary for its diagnosis. In a recent study of 769 patients with primary systemic amyloidosis, only 1% had confirmed symptomatic gastric amyloidosis. Amyloid deposition in the stomach can cause diffuse inflammation manifesting as a GI bleed, as in the case of our patient. Diagnosis requires biopsy with Congo red staining. Management and prognosis depend on the type and extent of deposition. Patients may require systemic therapy.
Disclosures:
Isha Samreen, MBBS, MPH1, Pooja Magavi, MD2, Ashwini Mulgaonkar, MD3, Rohit Khanna, DO4, Behnam Jahromi, MD2. P5137 - Gastrointestinal Amyloidosis: An Uncommon Cause of GI Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Hemet Global Medical Center, Murrieta, CA; 2Scripps Clinic, San Diego, CA; 3Scripps Green Hospital, La Jolla, CA; 4Scripps Green Hospital, San Diego, CA
Introduction: Systemic amyloidosis refers to a group of disorders characterized by misfolded protein deposition that can involve various organs. It is commonly associated with chronic inflammatory disorders, hematological malignancy and end-stage renal disease (ESRD). Gastrointestinal (GI) amyloidosis refers to the deposition of such proteins that in turn can interfere with the structure and function of GI organs, predominantly the liver and small bowel. We present a case of amyloidosis with gastric involvement.
Case Description/Methods: An 80-year-old Caucasian male with history of coronary artery disease, atrial fibrillation, Roux-en-Y gastric bypass (RYGB), ESRD on peritoneal dialysis and traumatic subdural hematoma initially presented to the emergency room after a fall with atrial fibrillation with rapid ventricular response, for which he was started on a heparin drip. He subsequently developed abdominal pain and melena, with a drop in hemoglobin from 8.5 to 7.9. mg/dL. Upper endoscopy showed evidence of bypass anatomy without active bleeding. However, the gastric mucosa was noted to be edematous with areas of friability and oozing on contact, and multiple cold forceps biopsies were obtained. Histological examination revealed abundant amyloid deposition in the lamina propria and blood vessels, confirmed with Congo red staining (Figure 1). The patient was ultimately diagnosed with AL amyloidosis with gastric involvement. He was evaluated by oncology, started on bortezemib and dexamethasone, and referred to cardiology in the setting of atrial fibrillation and elevated NT-proBNP for further cardiac evaluation. He was also presumed to have neurologic involvement manifesting as peripheral neuropathy and renal involvement worsening his ESRD.
Discussion: Gastrointestinal amyloidosis can present with nonspecific symptoms, including fatigue, abdominal pain and weight loss, mimicking other GI disorders. A high degree of clinical suspicion is necessary for its diagnosis. In a recent study of 769 patients with primary systemic amyloidosis, only 1% had confirmed symptomatic gastric amyloidosis. Amyloid deposition in the stomach can cause diffuse inflammation manifesting as a GI bleed, as in the case of our patient. Diagnosis requires biopsy with Congo red staining. Management and prognosis depend on the type and extent of deposition. Patients may require systemic therapy.
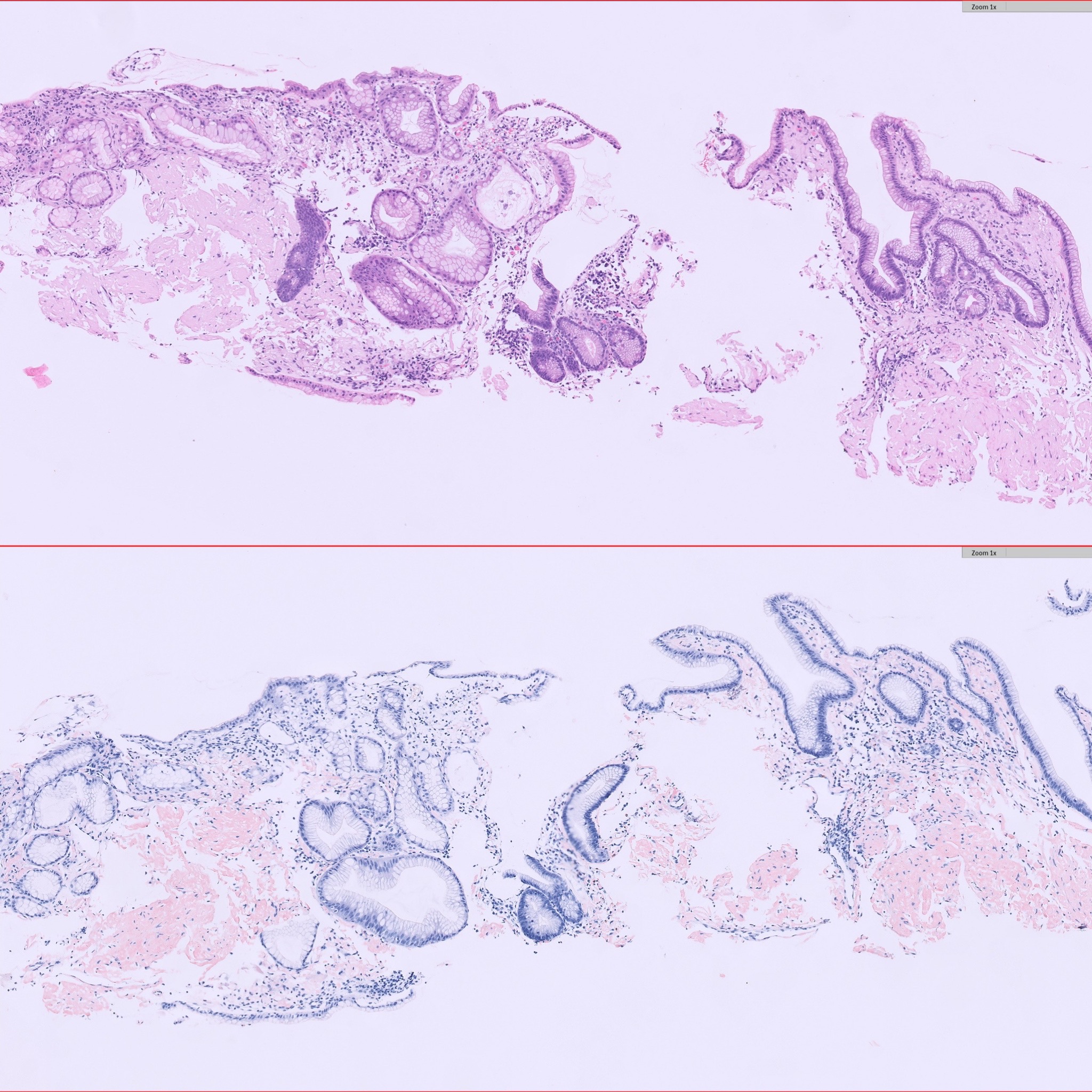
Figure: Figure 1
Disclosures:
Isha Samreen indicated no relevant financial relationships.
Pooja Magavi indicated no relevant financial relationships.
Ashwini Mulgaonkar indicated no relevant financial relationships.
Rohit Khanna indicated no relevant financial relationships.
Behnam Jahromi indicated no relevant financial relationships.
Isha Samreen, MBBS, MPH1, Pooja Magavi, MD2, Ashwini Mulgaonkar, MD3, Rohit Khanna, DO4, Behnam Jahromi, MD2. P5137 - Gastrointestinal Amyloidosis: An Uncommon Cause of GI Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
