Tuesday Poster Session
Category: Stomach
P5073 - Steroid Refractory Immune Checkpoint Inhibitor Induced Severe Gastritis Responsive to Infliximab
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MK
Michelle Kwon, MD
Brown University / Warren Alpert Medical School
Providence, RI
Presenting Author(s)
Michelle Kwon, MD1, Jacqueline J. Chu, MD1, Savan Kothadia, MD2, Fadlallah Habr, MD3
1Brown University / Warren Alpert Medical School, Providence, RI; 2Brown University / Lifespan Physician Group, Providence, RI; 3Rhode Island Hospital, Providence, RI
Introduction: Pembrolizumab, an immune checkpoint inhibitor (ICI) targeting PD-1, has been used since 2014 to treat various cancers. ICIs have been associated with colitis, but adverse effects in other areas of the gastrointestinal (GI) tract are far less prevalent. Here we describe a case of severe gastritis induced by pembrolizumab in a patient presenting with nausea and vomiting.
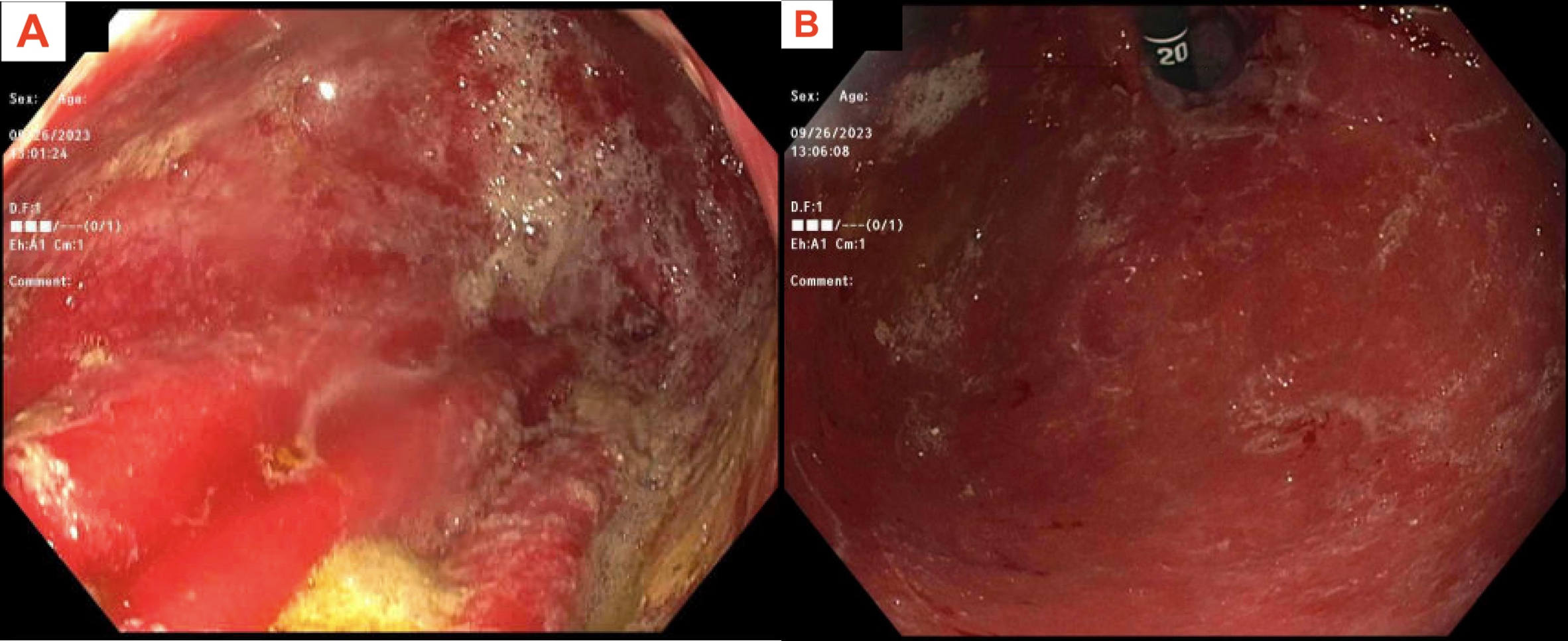
Case Description/Methods: A 44 year-old male with oropharyngeal carcinoma on pembrolizumab therapy for 2 years presented to the ED with weeks of poor oral intake and weight loss due to nausea and vomiting. He otherwise denied dysphagia, abdominal pain, odynophagia, hematemesis, melena, and hematochezia. Vital signs were suggestive of dehydration with tachycardia to 147 bpm and hypotension to 90/40 mmHg. Abdominal exam and labs were unremarkable except for mild hypokalemia (3.5). Subsequent esophagogastroduodenoscopy revealed diffuse severe inflammation characterized by erythema and friability in the entire visualized stomach (Image A,B). Histology from the gastric biopsies showed severe chronic active gastritis with diffuse ulceration and near complete destruction of the gastric mucosa. Given negative work up for infectious etiologies and lymphoproliferative disorders, the histologic findings were most consistent with severe pembrolizumab-induced gastritis. Subsequently, pembrolizumab was held and the patient was started on prednisone. Due to only mild symptom improvement with prednisone, infliximab 5 mg/kg was administered. The patient received two doses of infliximab, resulting in improved symptoms with subsequent tolerance to oral intake and gradual weight gain.
Discussion: While colitis is more commonly associated with ICIs including pembrolizumab, it is important to consider ICI involvement in other areas of the GI tract including the upper GI tract when patients on such therapies present with nonspecific GI symptoms and other etiologies are ruled out. Given that endoscopic evaluation often yields nonspecific findings like erythema and friability, histological evaluation with concurrent biochemical work up is necessary for definitive diagnosis. Treatment approaches, adapted from ICI-induced colitis management, include discontinuing the offending ICI and initiating steroids. If response to steroids is suboptimal, alternative agents such as infliximab can be considered. More investigation is required comparing how efficaciousness traditional treatment of ICI-induced colitis is in the setting of ICI-induced gastritis.
Disclosures:
Michelle Kwon, MD1, Jacqueline J. Chu, MD1, Savan Kothadia, MD2, Fadlallah Habr, MD3. P5073 - Steroid Refractory Immune Checkpoint Inhibitor Induced Severe Gastritis Responsive to Infliximab, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brown University / Warren Alpert Medical School, Providence, RI; 2Brown University / Lifespan Physician Group, Providence, RI; 3Rhode Island Hospital, Providence, RI
Introduction: Pembrolizumab, an immune checkpoint inhibitor (ICI) targeting PD-1, has been used since 2014 to treat various cancers. ICIs have been associated with colitis, but adverse effects in other areas of the gastrointestinal (GI) tract are far less prevalent. Here we describe a case of severe gastritis induced by pembrolizumab in a patient presenting with nausea and vomiting.
Case Description/Methods: A 44 year-old male with oropharyngeal carcinoma on pembrolizumab therapy for 2 years presented to the ED with weeks of poor oral intake and weight loss due to nausea and vomiting. He otherwise denied dysphagia, abdominal pain, odynophagia, hematemesis, melena, and hematochezia. Vital signs were suggestive of dehydration with tachycardia to 147 bpm and hypotension to 90/40 mmHg. Abdominal exam and labs were unremarkable except for mild hypokalemia (3.5). Subsequent esophagogastroduodenoscopy revealed diffuse severe inflammation characterized by erythema and friability in the entire visualized stomach (Image A,B). Histology from the gastric biopsies showed severe chronic active gastritis with diffuse ulceration and near complete destruction of the gastric mucosa. Given negative work up for infectious etiologies and lymphoproliferative disorders, the histologic findings were most consistent with severe pembrolizumab-induced gastritis. Subsequently, pembrolizumab was held and the patient was started on prednisone. Due to only mild symptom improvement with prednisone, infliximab 5 mg/kg was administered. The patient received two doses of infliximab, resulting in improved symptoms with subsequent tolerance to oral intake and gradual weight gain.
Discussion: While colitis is more commonly associated with ICIs including pembrolizumab, it is important to consider ICI involvement in other areas of the GI tract including the upper GI tract when patients on such therapies present with nonspecific GI symptoms and other etiologies are ruled out. Given that endoscopic evaluation often yields nonspecific findings like erythema and friability, histological evaluation with concurrent biochemical work up is necessary for definitive diagnosis. Treatment approaches, adapted from ICI-induced colitis management, include discontinuing the offending ICI and initiating steroids. If response to steroids is suboptimal, alternative agents such as infliximab can be considered. More investigation is required comparing how efficaciousness traditional treatment of ICI-induced colitis is in the setting of ICI-induced gastritis.
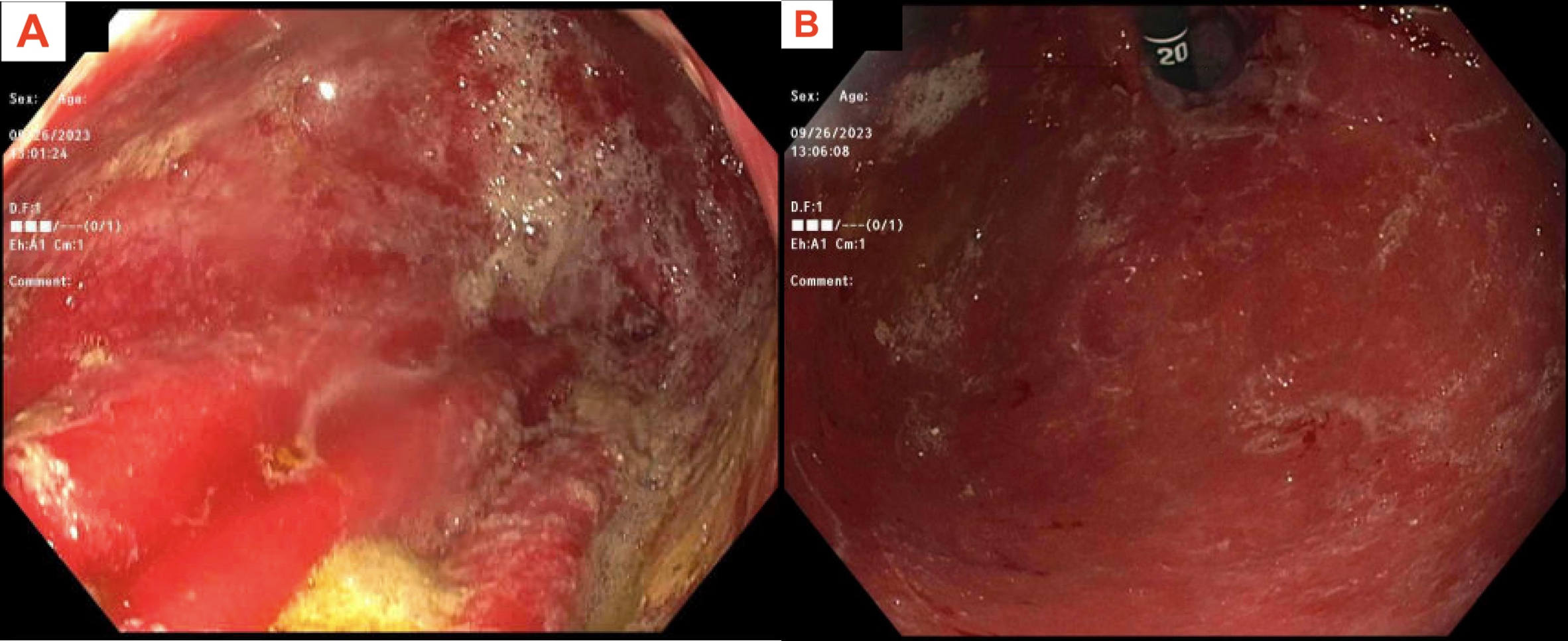
Figure: A: Gross endoscopic findings including severe, diffuse erythema with some ingested gastric contents. B: Similar diffuse erythema found in retroflexion.
Disclosures:
Michelle Kwon indicated no relevant financial relationships.
Jacqueline Chu indicated no relevant financial relationships.
Savan Kothadia indicated no relevant financial relationships.
Fadlallah Habr indicated no relevant financial relationships.
Michelle Kwon, MD1, Jacqueline J. Chu, MD1, Savan Kothadia, MD2, Fadlallah Habr, MD3. P5073 - Steroid Refractory Immune Checkpoint Inhibitor Induced Severe Gastritis Responsive to Infliximab, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
