Tuesday Poster Session
Category: Stomach
P5084 - Gastroparesis or Greater: A Case of Masked Adrenal Insufficiency
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jasmine Tidwell, MD
UConn John Dempsey Hospital
Hartford, CT
Presenting Author(s)
Jasmine Tidwell, MD1, Neil Khoury, MD2, Steven Goldenberg, MD2
1UConn John Dempsey Hospital, Hartford, CT; 2UConn Health, Hartford, CT
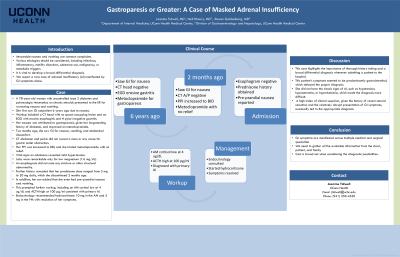
Introduction: Intractable nausea and vomiting are common complaints. Various etiologies should be considered, including infectious or inflammatory, motility disorders, substance use, malignancy, and metabolic triggers. It is vital to develop a broad differential diagnosis. We report a rare case of adrenal insufficiency (AI) manifested by GI symptoms alone.
Case Description/Methods: A 78-year-old woman with uncontrolled type 2 diabetes and polymyalgia rheumatica (PMR) on chronic steroids presented to the ER for worsening nausea and vomiting. She first saw GI outpatient six years ago due to nausea. Workup included a CT head with no space-occupying lesion and an EGD with erosive esophagitis and H pylori-negative gastritis. Her nausea was attributed to gastroparesis, given her longstanding history of diabetes, and improved on metoclopramide. Two months ago, she saw GI outpatient again for nausea, vomiting, and abdominal discomfort. CT abdomen and pelvis did not reveal a mass or any cause for gastric outlet obstruction. Her PPI was increased to BID, and she trialed metoclopramide with no relief. Vital signs on admission revealed mild hypertension. Labs were remarkable only for low magnesium (1.6 mg/dL). An esophagram did not note any stricture or other structural abnormality. Further history revealed that her prednisone ranged from 5 mg to 20 mg daily, which she discontinued two months ago. In addition, her son added that she even had pre-prandial nausea and vomiting. This prompted further workup, including an AM cortisol low at 4 ug/dL and ACTH elevated at 100 pg/ml consistent with secondary AI. Endocrinology recommended hydrocortisone 10 mg in the AM and 5 mg in the PM with resolution of her symptoms.
Discussion: This case highlights the importance of thorough history taking and a broad differential diagnosis whenever admitting a patient to the hospital. This patient’s symptoms seemed to be predominantly gastrointestinal, which delayed the proper diagnosis. She did not have the classic signs of AI, such as hypotension, hyponatremia, or hyperkalemia, which made the diagnosis more difficult. A high index of clinical suspicion, given the history of recent steroid cessation and the relatively abrupt presentation of GI symptoms, eventually led to the appropriate diagnosis. Overall, GI symptoms are manifested across multiple medical and surgical specialties, and we need to gather all the available information from the chart, patient, and family and cast a broad net when considering the diagnostic possibilities.
Disclosures:
Jasmine Tidwell, MD1, Neil Khoury, MD2, Steven Goldenberg, MD2. P5084 - Gastroparesis or Greater: A Case of Masked Adrenal Insufficiency, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1UConn John Dempsey Hospital, Hartford, CT; 2UConn Health, Hartford, CT
Introduction: Intractable nausea and vomiting are common complaints. Various etiologies should be considered, including infectious or inflammatory, motility disorders, substance use, malignancy, and metabolic triggers. It is vital to develop a broad differential diagnosis. We report a rare case of adrenal insufficiency (AI) manifested by GI symptoms alone.
Case Description/Methods: A 78-year-old woman with uncontrolled type 2 diabetes and polymyalgia rheumatica (PMR) on chronic steroids presented to the ER for worsening nausea and vomiting. She first saw GI outpatient six years ago due to nausea. Workup included a CT head with no space-occupying lesion and an EGD with erosive esophagitis and H pylori-negative gastritis. Her nausea was attributed to gastroparesis, given her longstanding history of diabetes, and improved on metoclopramide. Two months ago, she saw GI outpatient again for nausea, vomiting, and abdominal discomfort. CT abdomen and pelvis did not reveal a mass or any cause for gastric outlet obstruction. Her PPI was increased to BID, and she trialed metoclopramide with no relief. Vital signs on admission revealed mild hypertension. Labs were remarkable only for low magnesium (1.6 mg/dL). An esophagram did not note any stricture or other structural abnormality. Further history revealed that her prednisone ranged from 5 mg to 20 mg daily, which she discontinued two months ago. In addition, her son added that she even had pre-prandial nausea and vomiting. This prompted further workup, including an AM cortisol low at 4 ug/dL and ACTH elevated at 100 pg/ml consistent with secondary AI. Endocrinology recommended hydrocortisone 10 mg in the AM and 5 mg in the PM with resolution of her symptoms.
Discussion: This case highlights the importance of thorough history taking and a broad differential diagnosis whenever admitting a patient to the hospital. This patient’s symptoms seemed to be predominantly gastrointestinal, which delayed the proper diagnosis. She did not have the classic signs of AI, such as hypotension, hyponatremia, or hyperkalemia, which made the diagnosis more difficult. A high index of clinical suspicion, given the history of recent steroid cessation and the relatively abrupt presentation of GI symptoms, eventually led to the appropriate diagnosis. Overall, GI symptoms are manifested across multiple medical and surgical specialties, and we need to gather all the available information from the chart, patient, and family and cast a broad net when considering the diagnostic possibilities.
Disclosures:
Jasmine Tidwell indicated no relevant financial relationships.
Neil Khoury indicated no relevant financial relationships.
Steven Goldenberg indicated no relevant financial relationships.
Jasmine Tidwell, MD1, Neil Khoury, MD2, Steven Goldenberg, MD2. P5084 - Gastroparesis or Greater: A Case of Masked Adrenal Insufficiency, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
