Tuesday Poster Session
Category: Stomach
P5088 - A Rare Case of Primary Gastric Tuberculosis: Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Hasan Al-Obaidi, MD
Jamaica Hospital Medical Center
Briarwood, NY
Presenting Author(s)
Hasan Al-Obaidi, MD1, Pratiksha Moliya, MD2, Hussein Harb, 3, Iya Agha, MS4, Osamah Taher. Al-Obaidi, 5
1Jamaica Hospital Medical Center, Briarwood, NY; 2Jamaica Hospital Medical Center, Edison, NJ; 3Ross University School of Medicine, Brooklyn, NY; 4New York Institute of Technology College of Osteopathic Medicine, New York, NY; 5Al Qadisiyah University, Diwaniya, Al Qadisiyah, Iraq
Introduction: Tuberculosis (TB), historically termed "white death," is mainly caused by the Mycobacterium tuberculosis bacteria (MTB). Gastric TB is extremely rare, accounting for less than 0.2% of all TB cases.
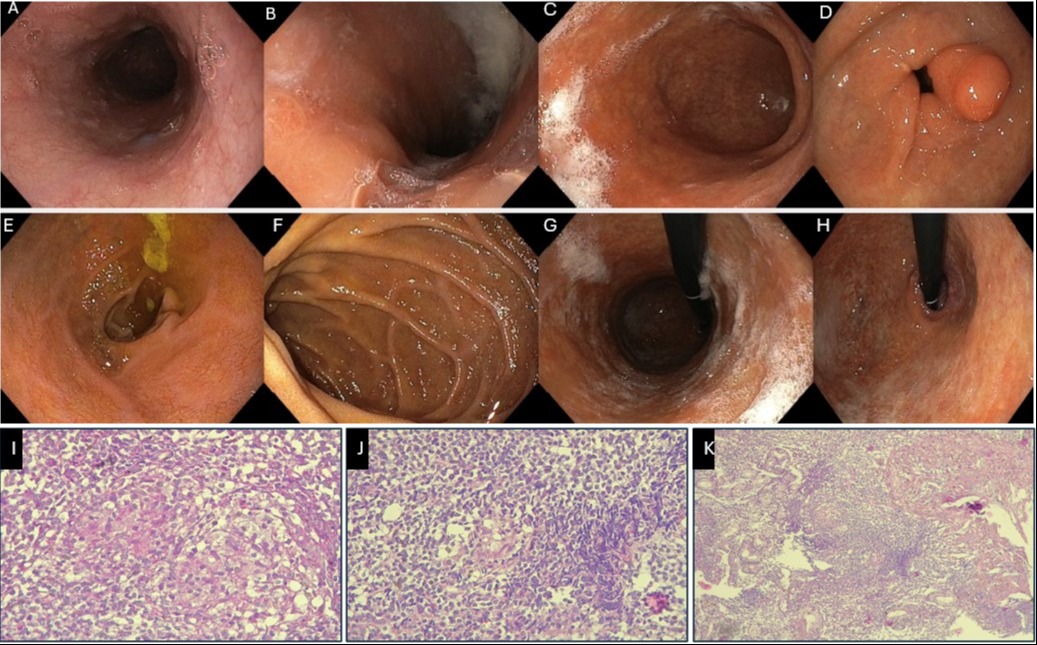
Case Description/Methods: A 50-year-old immunocompetent female from Iraq presented with three months of epigastric pain, accompanied by nausea, vomiting, and a nine-pound weight loss over the last two months. Examination showed mild epigastric tenderness. Lab results showed Hb: 10.2 g/dL, WBC: 5,900/µL, PLT: 280,000/µL, ESR: 11 mm/hr and normal liver enzymes. She tested negative for hepatitis and HIV. Chest X-ray and abdominal ultrasound were normal. Endoscopy showed a lax cardia, thickened mucosa, and a poorly distensible lumen. Biopsy of a subepithelial pyloric lesion revealed granulomas with multinucleated giant cells. CT chest and colonoscopy showed no additional findings. Pulmonary TB was ruled out, but the QuantiFERON test was positive, with normal serum ACE levels. Gastric TB was the primary diagnosis, with gastroduodenal Crohn's as an alternative. TB treatment was prioritized over Crohn's therapy to mitigate the risk of immunosuppression-induced TB flare-ups. She responded well, with symptoms improving rapidly. Three months later, she gained weight, and repeat endoscopy showed resolved lesions.
Discussion: Abdominal TB, constituting 1–3% of all cases and 12% of extrapulmonary cases, mainly affects the ileocecal region. Gastric TB is rarer due to stomach acidity and sparse lymphoid tissue, but it predominantly targets the prepyloric region, rich in lymph follicles. In our patient, MTB likely established infection through a subepithelial pyloric lesion, confirmed by biopsy. Endoscopic findings can mimic gastric cancer or peptic ulcer disease, often showing ulcers and hypertrophic masses. Biopsy yields are poor as TB granulomas reside in the submucosa. PCR can improve detection, though false negatives occur in 40%-65% of cases. Endoscopic USG is effective for characterizing TB lesions and obtaining cytological samples. Treatment involves isoniazid, rifampin, pyrazinamide, and ethambutol, akin to pulmonary TB therapy, which our patient responded well to. This case underscores the need for heightened clinical suspicion and aggressive diagnostic approaches, especially in patients with atypical abdominal symptoms, stressing the importance of early antitubercular therapy for favorable outcomes in rare manifestations.
Disclosures:
Hasan Al-Obaidi, MD1, Pratiksha Moliya, MD2, Hussein Harb, 3, Iya Agha, MS4, Osamah Taher. Al-Obaidi, 5. P5088 - A Rare Case of Primary Gastric Tuberculosis: Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jamaica Hospital Medical Center, Briarwood, NY; 2Jamaica Hospital Medical Center, Edison, NJ; 3Ross University School of Medicine, Brooklyn, NY; 4New York Institute of Technology College of Osteopathic Medicine, New York, NY; 5Al Qadisiyah University, Diwaniya, Al Qadisiyah, Iraq
Introduction: Tuberculosis (TB), historically termed "white death," is mainly caused by the Mycobacterium tuberculosis bacteria (MTB). Gastric TB is extremely rare, accounting for less than 0.2% of all TB cases.
Case Description/Methods: A 50-year-old immunocompetent female from Iraq presented with three months of epigastric pain, accompanied by nausea, vomiting, and a nine-pound weight loss over the last two months. Examination showed mild epigastric tenderness. Lab results showed Hb: 10.2 g/dL, WBC: 5,900/µL, PLT: 280,000/µL, ESR: 11 mm/hr and normal liver enzymes. She tested negative for hepatitis and HIV. Chest X-ray and abdominal ultrasound were normal. Endoscopy showed a lax cardia, thickened mucosa, and a poorly distensible lumen. Biopsy of a subepithelial pyloric lesion revealed granulomas with multinucleated giant cells. CT chest and colonoscopy showed no additional findings. Pulmonary TB was ruled out, but the QuantiFERON test was positive, with normal serum ACE levels. Gastric TB was the primary diagnosis, with gastroduodenal Crohn's as an alternative. TB treatment was prioritized over Crohn's therapy to mitigate the risk of immunosuppression-induced TB flare-ups. She responded well, with symptoms improving rapidly. Three months later, she gained weight, and repeat endoscopy showed resolved lesions.
Discussion: Abdominal TB, constituting 1–3% of all cases and 12% of extrapulmonary cases, mainly affects the ileocecal region. Gastric TB is rarer due to stomach acidity and sparse lymphoid tissue, but it predominantly targets the prepyloric region, rich in lymph follicles. In our patient, MTB likely established infection through a subepithelial pyloric lesion, confirmed by biopsy. Endoscopic findings can mimic gastric cancer or peptic ulcer disease, often showing ulcers and hypertrophic masses. Biopsy yields are poor as TB granulomas reside in the submucosa. PCR can improve detection, though false negatives occur in 40%-65% of cases. Endoscopic USG is effective for characterizing TB lesions and obtaining cytological samples. Treatment involves isoniazid, rifampin, pyrazinamide, and ethambutol, akin to pulmonary TB therapy, which our patient responded well to. This case underscores the need for heightened clinical suspicion and aggressive diagnostic approaches, especially in patients with atypical abdominal symptoms, stressing the importance of early antitubercular therapy for favorable outcomes in rare manifestations.
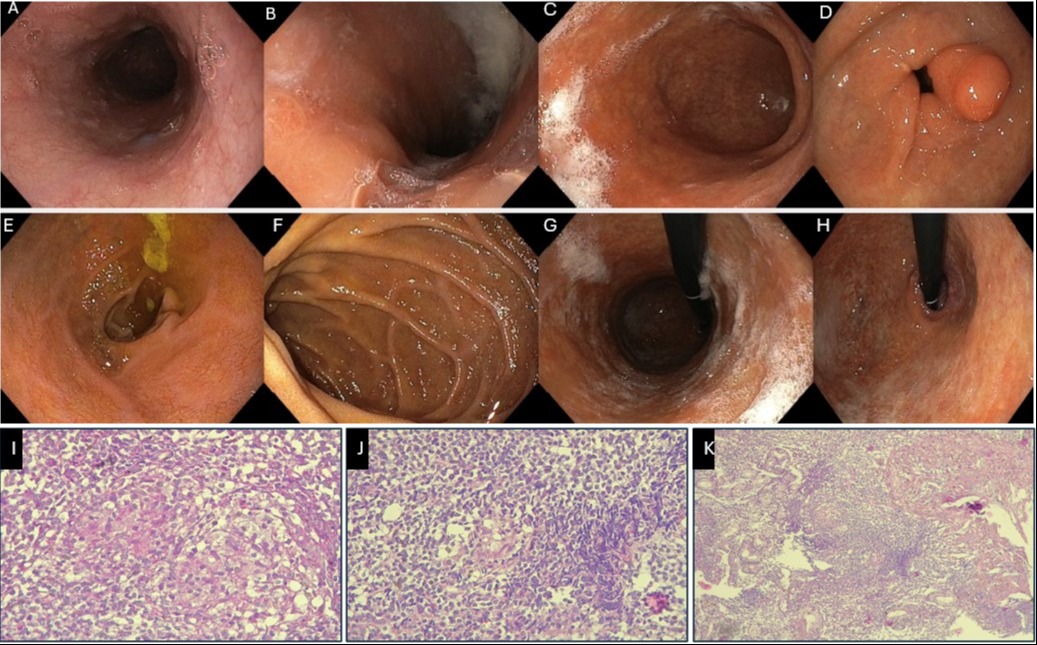
Figure: Figure1 (A,B,C,D,E,F,H): Upper endoscopy revealed a lax cardia, thickened mucosa, and a poorly distensible tube-like lumen at the cardia and body, with a subepithelial lesion at the pylorus.
Figure2 (I, J,K): Histopathology slides showing caseating granuloma.
Figure2 (I, J,K): Histopathology slides showing caseating granuloma.
Disclosures:
Hasan Al-Obaidi indicated no relevant financial relationships.
Pratiksha Moliya indicated no relevant financial relationships.
Hussein Harb indicated no relevant financial relationships.
Iya Agha indicated no relevant financial relationships.
Osamah Al-Obaidi indicated no relevant financial relationships.
Hasan Al-Obaidi, MD1, Pratiksha Moliya, MD2, Hussein Harb, 3, Iya Agha, MS4, Osamah Taher. Al-Obaidi, 5. P5088 - A Rare Case of Primary Gastric Tuberculosis: Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
