Tuesday Poster Session
Category: Practice Management
P4898 - Inadequate Implementation of Guideline-Directed Smoking Cessation Treatment in Common Gastrointestinal Disorders: Insights From a Learning Health System
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Brett D. Riederman, MD
Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital
St. Louis, MO
Presenting Author(s)
Brett D. Riederman, MD1, Li-Shiun Chen, MD, MPH, ScD2, Jingling Chen, BS3, Nina Smock, 2, Chien-Huan Chen, MD, PhD2
1Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, MO; 2Washington University School of Medicine in St. Louis, St. Louis, MO; 3Washington University School of Medicine, St. Louis, MO
Introduction: Tobacco smoking has been identified as a contributor to the development and progression of gastrointestinal (GI) disease as well as a risk factor for malignancy. As a result, many professional societies have included smoking cessation treatment such as medication and counseling as part of formal guidelines for management of many GI conditions. However, it is unclear how often this therapy is being provided. Therefore, we sought to evaluate smoking management among those with common diagnoses.
Methods: We queried the electronic health record database of a large academic healthcare system with ICD-10 codes to find all patients seen in clinics or hospitalized in 2023 for the most common GI diagnoses in the US.1 Diagnoses were then grouped as those with: current smoking cessation recommendations per professional societies (Group A), evidence for smoking harm but no formal recommendation (Group B), or neither evidence nor recommendations for smoking cessation (Group C). For each group and diagnosis, smoking prevalence was determined along with proportion receiving advice, medication, counseling offer, counseling referral, or any treatment.
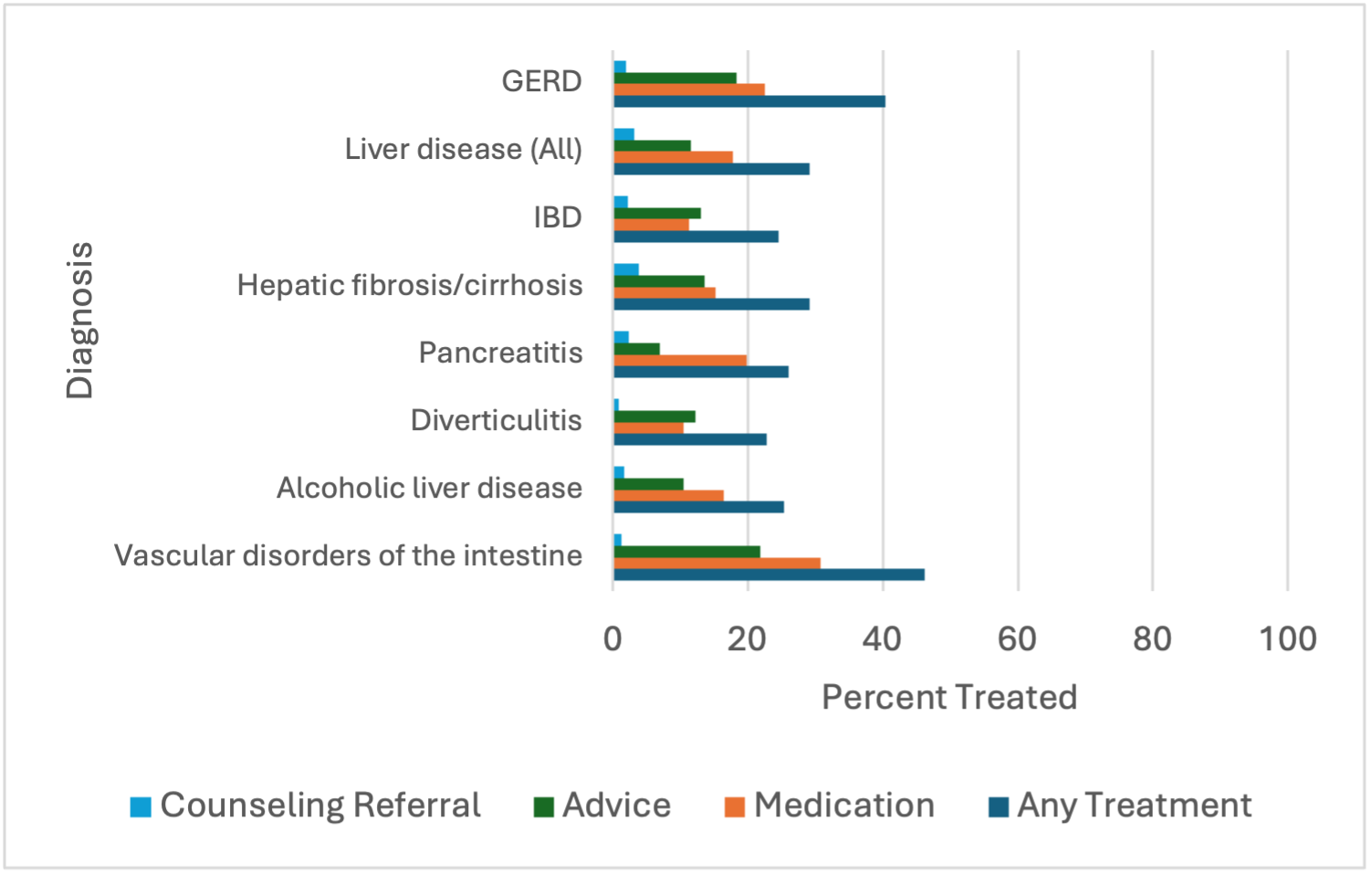
Results: 93361 subjects meeting criteria were assessed with 13715 identified as active smokers. Treatment numbers for Groups A, B, and C are listed in Table 1. Compared to Group C, patients in Group A have higher smoking prevalence (OR=1.30, 95% CI=1.23-1.37, p=0.0001) but no statistical difference in treatment rates (OR=0.923, 95% CI=0.83-1.04, p=0.18). Compared to Group C, Group B did not differ in rate of smoking (OR=1.14, 95% CI=0.99-1.32, p=0.07) or treatment (OR=0.93, 95% CI=0.71-1.23, p=0.61).
Discussion: Smoking cessation is important in managing at least 40% of the most common GI diagnoses. In our cohort, smoking prevalence was higher among those with society recommendations for tobacco treatment. However, treatment was not provided to these patients as per guidelines, potentially leading to worsened clinical outcomes. This inadequate application of guidelines may be a result of barriers in knowledge, implementation, support, or resources. Further study is warranted to determine how best to improve upon these metrics.
1. Peery AF, et al. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2021. Gastroenterology. 2022 Feb;162(2):621-644.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Brett D. Riederman, MD1, Li-Shiun Chen, MD, MPH, ScD2, Jingling Chen, BS3, Nina Smock, 2, Chien-Huan Chen, MD, PhD2. P4898 - Inadequate Implementation of Guideline-Directed Smoking Cessation Treatment in Common Gastrointestinal Disorders: Insights From a Learning Health System, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, MO; 2Washington University School of Medicine in St. Louis, St. Louis, MO; 3Washington University School of Medicine, St. Louis, MO
Introduction: Tobacco smoking has been identified as a contributor to the development and progression of gastrointestinal (GI) disease as well as a risk factor for malignancy. As a result, many professional societies have included smoking cessation treatment such as medication and counseling as part of formal guidelines for management of many GI conditions. However, it is unclear how often this therapy is being provided. Therefore, we sought to evaluate smoking management among those with common diagnoses.
Methods: We queried the electronic health record database of a large academic healthcare system with ICD-10 codes to find all patients seen in clinics or hospitalized in 2023 for the most common GI diagnoses in the US.1 Diagnoses were then grouped as those with: current smoking cessation recommendations per professional societies (Group A), evidence for smoking harm but no formal recommendation (Group B), or neither evidence nor recommendations for smoking cessation (Group C). For each group and diagnosis, smoking prevalence was determined along with proportion receiving advice, medication, counseling offer, counseling referral, or any treatment.
Results: 93361 subjects meeting criteria were assessed with 13715 identified as active smokers. Treatment numbers for Groups A, B, and C are listed in Table 1. Compared to Group C, patients in Group A have higher smoking prevalence (OR=1.30, 95% CI=1.23-1.37, p=0.0001) but no statistical difference in treatment rates (OR=0.923, 95% CI=0.83-1.04, p=0.18). Compared to Group C, Group B did not differ in rate of smoking (OR=1.14, 95% CI=0.99-1.32, p=0.07) or treatment (OR=0.93, 95% CI=0.71-1.23, p=0.61).
Discussion: Smoking cessation is important in managing at least 40% of the most common GI diagnoses. In our cohort, smoking prevalence was higher among those with society recommendations for tobacco treatment. However, treatment was not provided to these patients as per guidelines, potentially leading to worsened clinical outcomes. This inadequate application of guidelines may be a result of barriers in knowledge, implementation, support, or resources. Further study is warranted to determine how best to improve upon these metrics.
1. Peery AF, et al. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2021. Gastroenterology. 2022 Feb;162(2):621-644.
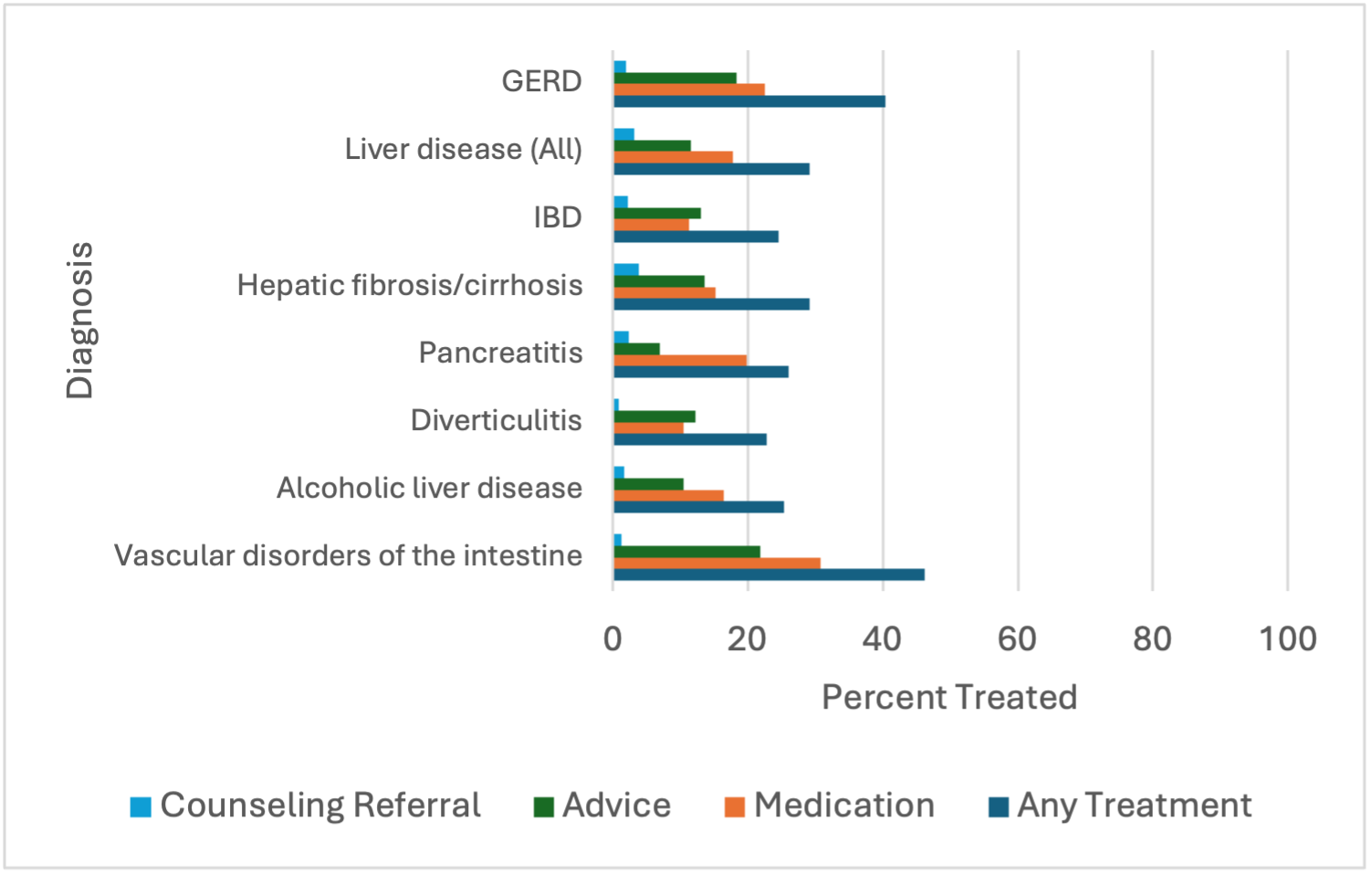
Figure: Figure 1. Frequency of guideline-directed smoking treatment for Group A diagnoses
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Brett Riederman indicated no relevant financial relationships.
Li-Shiun Chen indicated no relevant financial relationships.
Jingling Chen indicated no relevant financial relationships.
Nina Smock indicated no relevant financial relationships.
Chien-Huan Chen indicated no relevant financial relationships.
Brett D. Riederman, MD1, Li-Shiun Chen, MD, MPH, ScD2, Jingling Chen, BS3, Nina Smock, 2, Chien-Huan Chen, MD, PhD2. P4898 - Inadequate Implementation of Guideline-Directed Smoking Cessation Treatment in Common Gastrointestinal Disorders: Insights From a Learning Health System, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
