Tuesday Poster Session
Category: Liver
P4812 - Poor Diagnosis Leads to Poor Prognosis: Dramatic Presentation of Occult Cirrhosis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Zainab Mujahid, MD
University of Maryland Capital Region Health
Lorton, VA
Presenting Author(s)
Zainab Mujahid, MD1, Saeed Shoar, MD2, Mohammed Rifat Shaik, MBBS3, Homayoon Mahjoob, MD, MPH4, Asghar Shaigany, MD2
1University of Maryland Capital Region Medical Center, Lorton, VA; 2University of Maryland Capital Region Health, Largo, MD; 3University of Maryland Medical Center Midtown Campus, Baltimore, MD; 4University of Maryland Capital Region Medical Center, Largo, MD
Introduction: Metabolic associated steatotic liver disease (MASLD) contributes up to 25% of cirrhosis. The interval between disease acquisition and development of cirrhosis is overlooked on routine workup in asymptomatic patients. Diagnosis requires careful evaluation of clinical co-morbidities. Utilization of noninvasive tools such as fatty liver index (FLI) to determine which patients warrant further workup is key in early intervention. Here we describe a case of fulminant hepatic failure in a patient with occult cirrhosis secondary to MASLD.
Case Description/Methods: A 56 yof with a PMH of HTN, HLD, diabetes, and obesity BMI 31, w/no PMH of alcohol use disorder presented with profuse hematemesis. Vitals at presentation BP 99/49, HR 125, 96% on 3L. Became lethargic in the ED requiring intubation for airway protection. Lab work was significant for Hb 6.5g/dL, platelets 125k, ast/alt 52/30UL, albumin 2.6g/dL, INR 1.8, and HbA1c 7.6.
Workup revealed antiSMA 1:20, negative hepatitis panel, no prior abnormal LFTs. She followed regularly with her PCP and was seen 10 days prior to hospitalization. Relevant outpatient labs were ALK- 146s, Plt-134k, AST/ALT 23/27.
Following resuscitation with pRBC and FFP EGD was performed, it was significant for grade III esophageal varices, banded. Course was complicated by multiorgan failure, shock, and persistent encephalopathy. Due to unrestored mentation the patient was not transferred to a tertiary center. Her code status was changed to comfort care on hospital day 6, she expired soon after.
Discussion: MAFLD affects up to 30% of adults in the general population, nearly one third of these patients progress to steatotic liver disease (SLD) and subsequently cirrhosis.
Early screening of patients with metabolic syndrome phenotype would expedite the diagnosis, as mortality is significantly increased in patients with comorbidities. The highest mortality was seen with co-existing MALSD-SLD (aHR 1.32), this risk was further compounded in diabetics (aHR 1.68), with the highest mortality seen in patients with MASLD-SLD with liver fibrosis (aHR 2.29) Metabolism ‘24, such as our unfortunate patient.
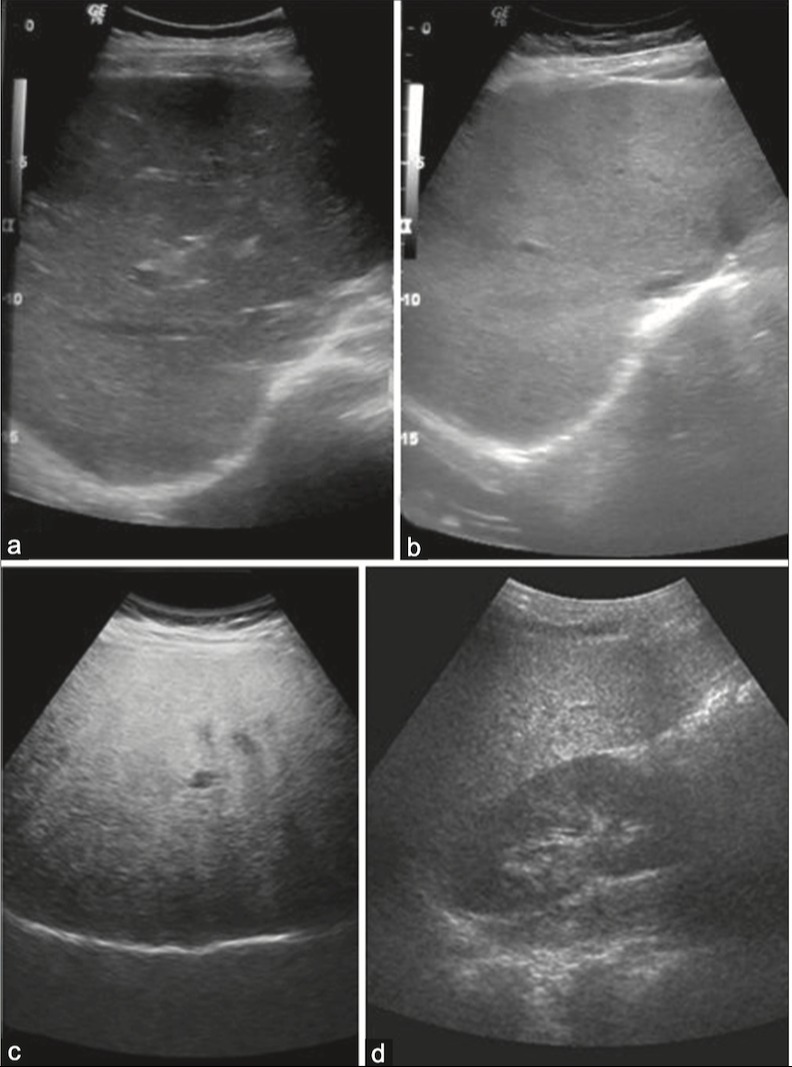
Scoring systems such as FLI takes into account BMI, waist circumference, LAE, and GGT. Imaging options include abdominal US with increased sensitivity of up to 90% in biopsy proven steatosis >20%, World J Gastro ‘14. Advances in noninvasive diagnostic methods is the key in bridging the gap between primary care and gastroenterology in this rapidly growing patient population.
Disclosures:
Zainab Mujahid, MD1, Saeed Shoar, MD2, Mohammed Rifat Shaik, MBBS3, Homayoon Mahjoob, MD, MPH4, Asghar Shaigany, MD2. P4812 - Poor Diagnosis Leads to Poor Prognosis: Dramatic Presentation of Occult Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Maryland Capital Region Medical Center, Lorton, VA; 2University of Maryland Capital Region Health, Largo, MD; 3University of Maryland Medical Center Midtown Campus, Baltimore, MD; 4University of Maryland Capital Region Medical Center, Largo, MD
Introduction: Metabolic associated steatotic liver disease (MASLD) contributes up to 25% of cirrhosis. The interval between disease acquisition and development of cirrhosis is overlooked on routine workup in asymptomatic patients. Diagnosis requires careful evaluation of clinical co-morbidities. Utilization of noninvasive tools such as fatty liver index (FLI) to determine which patients warrant further workup is key in early intervention. Here we describe a case of fulminant hepatic failure in a patient with occult cirrhosis secondary to MASLD.
Case Description/Methods: A 56 yof with a PMH of HTN, HLD, diabetes, and obesity BMI 31, w/no PMH of alcohol use disorder presented with profuse hematemesis. Vitals at presentation BP 99/49, HR 125, 96% on 3L. Became lethargic in the ED requiring intubation for airway protection. Lab work was significant for Hb 6.5g/dL, platelets 125k, ast/alt 52/30UL, albumin 2.6g/dL, INR 1.8, and HbA1c 7.6.
Workup revealed antiSMA 1:20, negative hepatitis panel, no prior abnormal LFTs. She followed regularly with her PCP and was seen 10 days prior to hospitalization. Relevant outpatient labs were ALK- 146s, Plt-134k, AST/ALT 23/27.
Following resuscitation with pRBC and FFP EGD was performed, it was significant for grade III esophageal varices, banded. Course was complicated by multiorgan failure, shock, and persistent encephalopathy. Due to unrestored mentation the patient was not transferred to a tertiary center. Her code status was changed to comfort care on hospital day 6, she expired soon after.
Discussion: MAFLD affects up to 30% of adults in the general population, nearly one third of these patients progress to steatotic liver disease (SLD) and subsequently cirrhosis.
Early screening of patients with metabolic syndrome phenotype would expedite the diagnosis, as mortality is significantly increased in patients with comorbidities. The highest mortality was seen with co-existing MALSD-SLD (aHR 1.32), this risk was further compounded in diabetics (aHR 1.68), with the highest mortality seen in patients with MASLD-SLD with liver fibrosis (aHR 2.29) Metabolism ‘24, such as our unfortunate patient.
Scoring systems such as FLI takes into account BMI, waist circumference, LAE, and GGT. Imaging options include abdominal US with increased sensitivity of up to 90% in biopsy proven steatosis >20%, World J Gastro ‘14. Advances in noninvasive diagnostic methods is the key in bridging the gap between primary care and gastroenterology in this rapidly growing patient population.
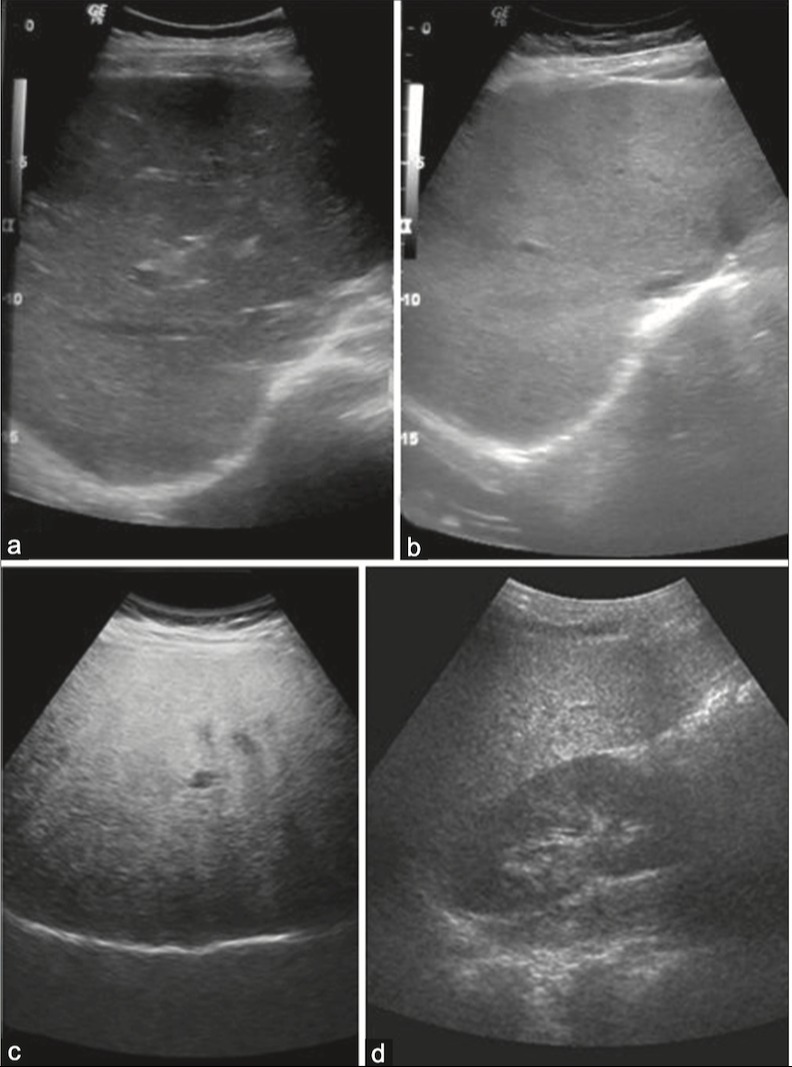
Figure: Grade of Fatty Liver on Ultrasound; A) Normal liver echogenicity B) Grade 1 Mild increase in echogenicity C) Grade 2 Moderate increase echogenicity with impaired visualization of diaphragm D) Severe increase in echogenicity with impaired visualization of portal vein wall and diaphragm is obscured.
Disclosures:
Zainab Mujahid indicated no relevant financial relationships.
Saeed Shoar indicated no relevant financial relationships.
Mohammed Rifat Shaik indicated no relevant financial relationships.
Homayoon Mahjoob indicated no relevant financial relationships.
Asghar Shaigany indicated no relevant financial relationships.
Zainab Mujahid, MD1, Saeed Shoar, MD2, Mohammed Rifat Shaik, MBBS3, Homayoon Mahjoob, MD, MPH4, Asghar Shaigany, MD2. P4812 - Poor Diagnosis Leads to Poor Prognosis: Dramatic Presentation of Occult Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
