Tuesday Poster Session
Category: Liver
P4816 - T-Cell-Induced Porto-Sinusoidal Vascular Disorder (PSVD)
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- MT
Manaswitha Thota, MD
Virginia Commonwealth University Medical Center
Richmond, VA
Presenting Author(s)
Manaswitha Thota, MD1, Vihitha Thota, MD2
1Virginia Commonwealth University Medical Center, Richmond, VA; 2University of Texas Medical Branch, Galveston, TX
Introduction: Pathophysiology of PSVD, a rare underdiagnosed disease, is not well understood. We present a case of a healthy patient with pancytopenia who was diagnosed with PSVD, with pathologic findings highlighting a potential cause of the disease.
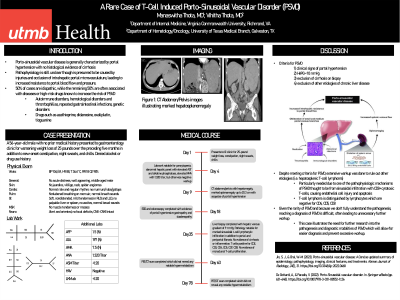
Case Description/Methods: A 56-year-old male with no prior medical history presented to gastroenterology clinic for worsening weight loss of 25 pounds over five months in addition to new-onset constipation, night sweats, and chills. He denied alcohol or drug use history. Laboratory tests revealed pancytopenia with white blood cell count (WBC) 1730/uL with absolute neutrophil count of 600/uL, hemoglobin 7.9 g/dL, and platelet count 57,000/uL in addition to elevated AST 53U/L and alkaline phosphatase 191U/L. ANA was 1:320 with otherwise negative work-up for autoimmune, infectious, and hypercoagulable etiologies. CT abdomen/pelvis showed hepatomegaly with hypodensities identified as cysts, marked splenomegaly up to 20.3cm with sequelae of portal hypertension. Given anemia, EGD and colonoscopy were done, with evidence of portal hypertensive gastropathy and duodenopathy. Over the next several months, patient underwent further work-up, including a liver biopsy with hepatic venous pressure gradient (HVPG) of 9 mmHg; pathology showed marked sinusoidal t-cell lymphocytic cell infiltration in addition to portal and periportal fibrosis without evidence of cirrhosis or inflammation. T-cells were positive for CD2, CD3, CD4, CD5, CD7 (weak), and CD8; there was no evidence of monoclonal T-cell proliferation on further testing. In order to definitively rule out T-cell lymphoma, PET/CT was done which did not reveal notable hypermetabolism, including in the liver. Subsequent bone marrow biopsy showed a normocellular marrow without evidence of neoplasm.
Discussion: Our patient met the criteria for PSVD: clinical signs of portal hypertension, HVPG < 10 mmHg, exclusion of cirrhosis on biopsy, and exclusion of other etiologies of chronic liver disease. However, extensive work-up was done to rule out other etiologies, particularly hematologic causes like hepatosplenic T-cell lymphoma. This diagnostic dilemma arises due to one of the pathophysiologic mechanisms of PSVD thought to be from sinusoidal infiltration with CD8+ cytotoxic T-cells, causing endothelial injury and apoptosis. T-cell lymphoma is distinguished by lymphocytes which are negative for CD4, CD5, and CD8. This case highlights the need for further research into the pathogenesis and diagnostic modalities of this disease.
Disclosures:
Manaswitha Thota, MD1, Vihitha Thota, MD2. P4816 - T-Cell-Induced Porto-Sinusoidal Vascular Disorder (PSVD), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Virginia Commonwealth University Medical Center, Richmond, VA; 2University of Texas Medical Branch, Galveston, TX
Introduction: Pathophysiology of PSVD, a rare underdiagnosed disease, is not well understood. We present a case of a healthy patient with pancytopenia who was diagnosed with PSVD, with pathologic findings highlighting a potential cause of the disease.
Case Description/Methods: A 56-year-old male with no prior medical history presented to gastroenterology clinic for worsening weight loss of 25 pounds over five months in addition to new-onset constipation, night sweats, and chills. He denied alcohol or drug use history. Laboratory tests revealed pancytopenia with white blood cell count (WBC) 1730/uL with absolute neutrophil count of 600/uL, hemoglobin 7.9 g/dL, and platelet count 57,000/uL in addition to elevated AST 53U/L and alkaline phosphatase 191U/L. ANA was 1:320 with otherwise negative work-up for autoimmune, infectious, and hypercoagulable etiologies. CT abdomen/pelvis showed hepatomegaly with hypodensities identified as cysts, marked splenomegaly up to 20.3cm with sequelae of portal hypertension. Given anemia, EGD and colonoscopy were done, with evidence of portal hypertensive gastropathy and duodenopathy. Over the next several months, patient underwent further work-up, including a liver biopsy with hepatic venous pressure gradient (HVPG) of 9 mmHg; pathology showed marked sinusoidal t-cell lymphocytic cell infiltration in addition to portal and periportal fibrosis without evidence of cirrhosis or inflammation. T-cells were positive for CD2, CD3, CD4, CD5, CD7 (weak), and CD8; there was no evidence of monoclonal T-cell proliferation on further testing. In order to definitively rule out T-cell lymphoma, PET/CT was done which did not reveal notable hypermetabolism, including in the liver. Subsequent bone marrow biopsy showed a normocellular marrow without evidence of neoplasm.
Discussion: Our patient met the criteria for PSVD: clinical signs of portal hypertension, HVPG < 10 mmHg, exclusion of cirrhosis on biopsy, and exclusion of other etiologies of chronic liver disease. However, extensive work-up was done to rule out other etiologies, particularly hematologic causes like hepatosplenic T-cell lymphoma. This diagnostic dilemma arises due to one of the pathophysiologic mechanisms of PSVD thought to be from sinusoidal infiltration with CD8+ cytotoxic T-cells, causing endothelial injury and apoptosis. T-cell lymphoma is distinguished by lymphocytes which are negative for CD4, CD5, and CD8. This case highlights the need for further research into the pathogenesis and diagnostic modalities of this disease.
Disclosures:
Manaswitha Thota indicated no relevant financial relationships.
Vihitha Thota indicated no relevant financial relationships.
Manaswitha Thota, MD1, Vihitha Thota, MD2. P4816 - T-Cell-Induced Porto-Sinusoidal Vascular Disorder (PSVD), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
