Tuesday Poster Session
Category: Liver
P4829 - Sigmoid Diverticulitis Presenting as Pyogenic Liver Abscess
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SA
Shuhaib Ali, DO
University of Texas Health Science Center
San Antonio, TX
Presenting Author(s)
Shuhaib Ali, DO1, Ziyyan Ali, BA2, Farah Hadi. Ladak, MD3, Umesha Naragalu, MD4
1University of Texas Health Science Center, San Antonio, TX; 2University of the Incarnate Word, San Antonio, TX; 3Audie Murphy VA Hospital, San Antonio, TX; 4University of Texas Health San Antonio, San Antonio, TX
Introduction: Pyogenic liver abscess (PLA) can be an uncommon manifestation of hepatobiliary disease, intra-abdominal infection, abdominal surgery, liver transplant, or liver trauma. We present a rare case of hepatic PLA as a preceding presentation of acute sigmoid diverticulitis.
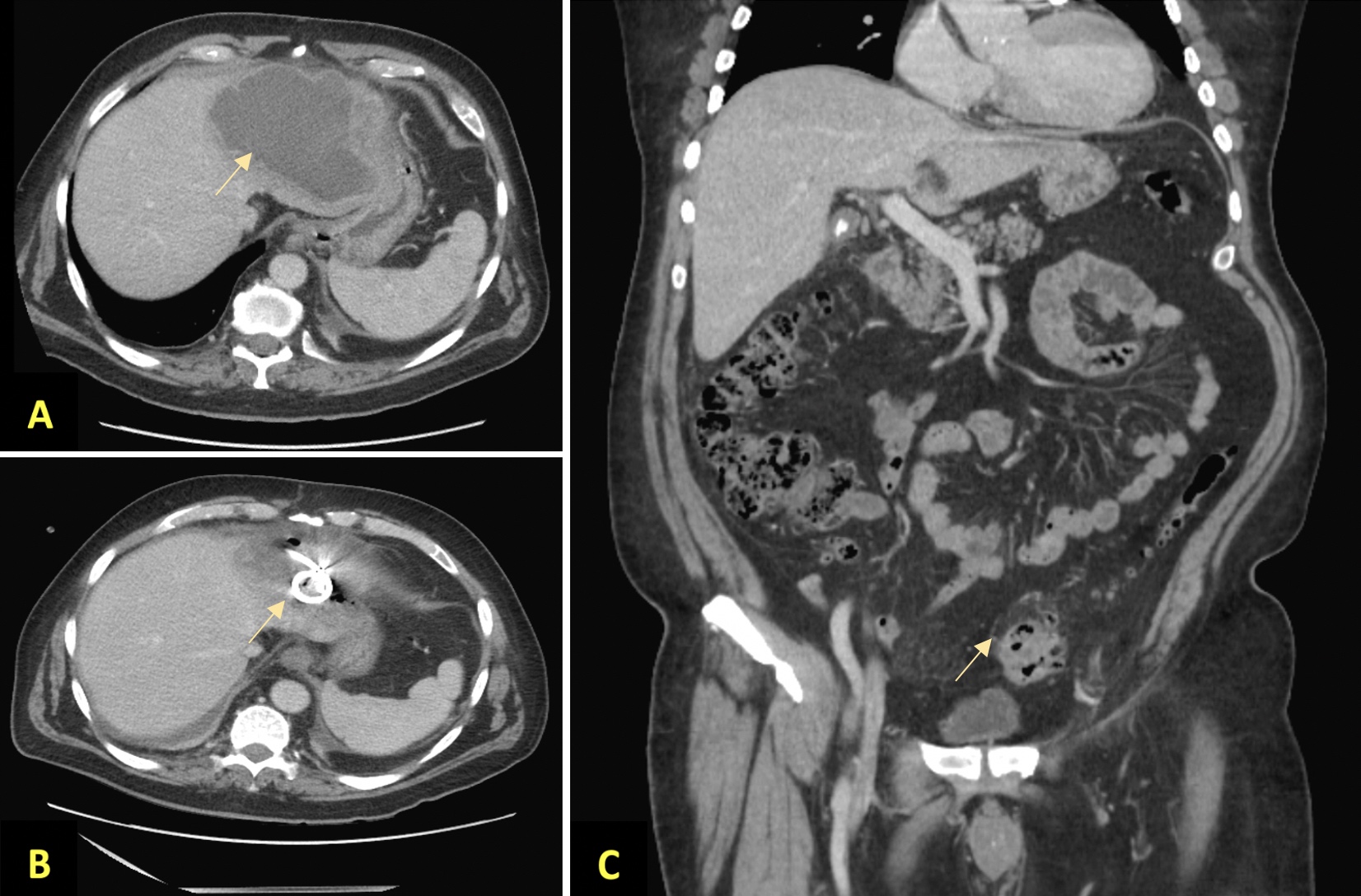
Case Description/Methods: A 66 year-old man with coronary artery disease, recent diagnosis of pulmonary embolism on anticoagulation presented with fever up to 101°F, chills, and night sweats. Other vital signs were within normal limits. The patient denied recent travel or dental work. Labs were pertinent for leukocytosis to 26.5 x 103/uL, elevated total bilirubin (2.3 mg/dL), alkaline phosphatase (537 IU/L), aspartate transaminase (40 IU/L), and alanine transaminase (69 IU/L). Computed tomography of the abdomen and pelvis (CT A/P) revealed a left hepatic lobe abscess measuring 14 cm, colonic diverticulosis, and cholelithiasis without evidence of cholecystitis. Blood cultures were negative. Serological tests for Entamoeba histolytica antibody, Human immunodeficiency virus, and Hepatitis C panels were negative. Transthoracic echocardiogram did not show evidence of endocarditis. Drainage of the hepatic abscess revealed purulent drainage with fluid culture growing Streptococcus anginosus and Fusobacterium nucleatum. He was initially treated with piperacillin-tazobactam. A follow-up CT A/P showed a decrease in the size of the hepatic abscess to 7 cm with drainage, however, the imaging also revealed peri-sigmoid fat stranding consistent with sigmoid diverticulitis and small intramural abscess, confirming the source of the PLA. The patient was discharged on amoxicillin-clavulanate for six weeks. Follow-up imaging two months later confirmed resolution of the liver abscess. The patient is pending colonoscopy as an outpatient.
Discussion: We present a rare case of polymicrobial PLA as a complication of acute diverticulitis which is unique as the hepatic abscess preceded the presentation of diverticulitis by several days. To our knowledge, only a few cases have been reported of hepatic abscess preceding the presentation of diverticulitis. Colonic mucosal disruption in the setting of active inflammation allows bacterial translocation to the portal venous system and ultimately to the liver resulting in liver abcess. This case highlights the importance identifying the underlying source of the hepatic abscess. Though rare, diverticulitis as a source of pyogenic liver abscess should be considered.
Disclosures:
Shuhaib Ali, DO1, Ziyyan Ali, BA2, Farah Hadi. Ladak, MD3, Umesha Naragalu, MD4. P4829 - Sigmoid Diverticulitis Presenting as Pyogenic Liver Abscess, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health Science Center, San Antonio, TX; 2University of the Incarnate Word, San Antonio, TX; 3Audie Murphy VA Hospital, San Antonio, TX; 4University of Texas Health San Antonio, San Antonio, TX
Introduction: Pyogenic liver abscess (PLA) can be an uncommon manifestation of hepatobiliary disease, intra-abdominal infection, abdominal surgery, liver transplant, or liver trauma. We present a rare case of hepatic PLA as a preceding presentation of acute sigmoid diverticulitis.
Case Description/Methods: A 66 year-old man with coronary artery disease, recent diagnosis of pulmonary embolism on anticoagulation presented with fever up to 101°F, chills, and night sweats. Other vital signs were within normal limits. The patient denied recent travel or dental work. Labs were pertinent for leukocytosis to 26.5 x 103/uL, elevated total bilirubin (2.3 mg/dL), alkaline phosphatase (537 IU/L), aspartate transaminase (40 IU/L), and alanine transaminase (69 IU/L). Computed tomography of the abdomen and pelvis (CT A/P) revealed a left hepatic lobe abscess measuring 14 cm, colonic diverticulosis, and cholelithiasis without evidence of cholecystitis. Blood cultures were negative. Serological tests for Entamoeba histolytica antibody, Human immunodeficiency virus, and Hepatitis C panels were negative. Transthoracic echocardiogram did not show evidence of endocarditis. Drainage of the hepatic abscess revealed purulent drainage with fluid culture growing Streptococcus anginosus and Fusobacterium nucleatum. He was initially treated with piperacillin-tazobactam. A follow-up CT A/P showed a decrease in the size of the hepatic abscess to 7 cm with drainage, however, the imaging also revealed peri-sigmoid fat stranding consistent with sigmoid diverticulitis and small intramural abscess, confirming the source of the PLA. The patient was discharged on amoxicillin-clavulanate for six weeks. Follow-up imaging two months later confirmed resolution of the liver abscess. The patient is pending colonoscopy as an outpatient.
Discussion: We present a rare case of polymicrobial PLA as a complication of acute diverticulitis which is unique as the hepatic abscess preceded the presentation of diverticulitis by several days. To our knowledge, only a few cases have been reported of hepatic abscess preceding the presentation of diverticulitis. Colonic mucosal disruption in the setting of active inflammation allows bacterial translocation to the portal venous system and ultimately to the liver resulting in liver abcess. This case highlights the importance identifying the underlying source of the hepatic abscess. Though rare, diverticulitis as a source of pyogenic liver abscess should be considered.
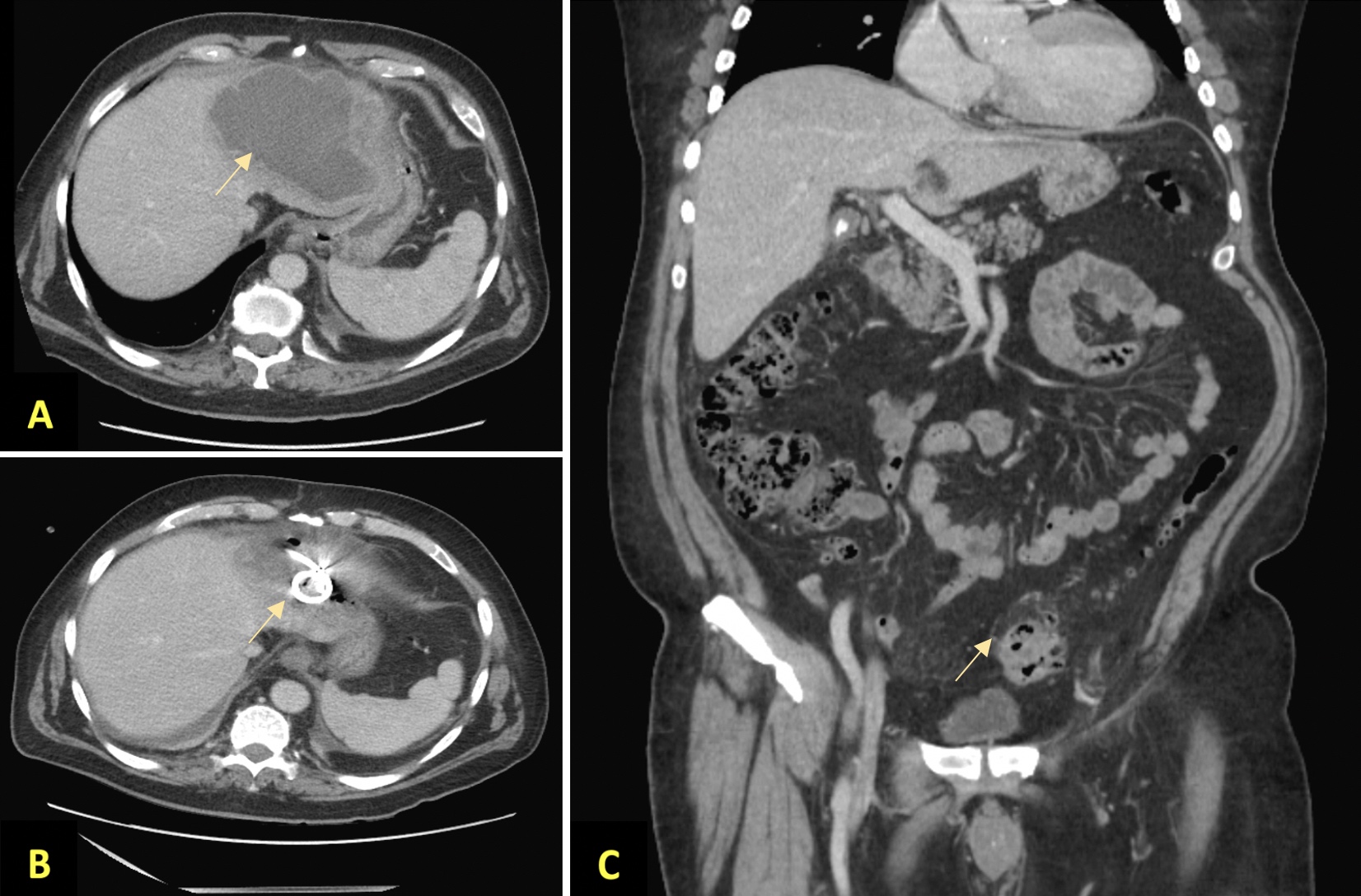
Figure: A. CT abdomen and pelvis findings with pyogenic hepatic abscess on admission
B. Follow up CT abdomen and pelvis showing decreased size of hepatic abscess status post drain placement
C. Follow up CT abdomen and pelvis revealed peri-sigmoid fat stranding consistent with sigmoid diverticulitis and small intramural abscess.
B. Follow up CT abdomen and pelvis showing decreased size of hepatic abscess status post drain placement
C. Follow up CT abdomen and pelvis revealed peri-sigmoid fat stranding consistent with sigmoid diverticulitis and small intramural abscess.
Disclosures:
Shuhaib Ali indicated no relevant financial relationships.
Ziyyan Ali indicated no relevant financial relationships.
Farah Ladak indicated no relevant financial relationships.
Umesha Naragalu indicated no relevant financial relationships.
Shuhaib Ali, DO1, Ziyyan Ali, BA2, Farah Hadi. Ladak, MD3, Umesha Naragalu, MD4. P4829 - Sigmoid Diverticulitis Presenting as Pyogenic Liver Abscess, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
