Tuesday Poster Session
Category: Liver
P4748 - Metastatic Breast Cancer in a Liver Transplant Patient Originating From the Cadaver Donor
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Smriti Kochhar, DO
Penn State Health Milton S. Hershey Medical Center
Hershey, PA
Presenting Author(s)
Smriti Kochhar, DO1, Amee Pansuriya, DO1, Curtis McInnis, DO1, Fnu Anamika, MBBS2, Rohit Jain, MD1
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2Delhi, Hershey, PA
Introduction: There is a 0.4% incidence of new post-transplant solid tumors in the United States. Malignancies in solid organ transplant recipients (SOTR) are concerning because these patients typically have a poor prognosis compared to the general population. Living donor screening involves a comprehensive review of the donor's medical history and physical examination, while deceased donor screening also involves testing for tumor markers. However, there is no universal protocol for cancer screening for solid organ transplants, and a few cases of cancer in SOTR have been reported. We present a case of a 58-year-old female who developed metastatic breast cancer from a transplanted donor liver.
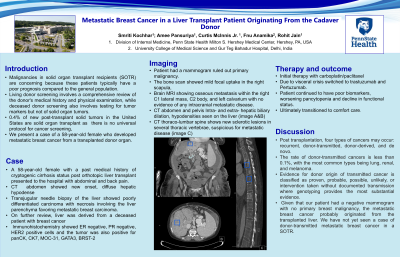
Case Description/Methods: A 58-year-old female with a past medical history of cryptogenic cirrhosis status post orthotopic liver transplant one year ago (from a deceased breast cancer patient) on immunosuppression with tacrolimus and prednisone came to the hospital with abdominal and back pain. A CT abdomen showed new onset, diffuse hepatic hypodense lesions in the upper lobe, and a transjugular needle biopsy of the liver showed poorly differentiated carcinoma with necrosis involving the liver parenchyma, favoring metastatic breast carcinoma. Immunohistochemistry showed ER negative, PR-negative, and HER2 positive cells, and the tumor was also positive for panCK, CK7, MOC-31, GATA3, BRST-2 however, additional work-up with a mammogram ruled out primary malignancy. The bone scan showed mild focal uptake in the right scapula, with a brain MRI showing osseous metastasis within the right C1 lateral mass, C2 body, and left calvarium with no evidence of any intracranial metastatic disease. Systemic therapy with carboplatin/paclitaxel was initiated due to potential visceral crisis.
Discussion: Post transplantation, four types of cancers may occur: recurrent, donor-transmitted, donor-derived, and de novo. The rate of donor-transmitted cancers is less than 0.1%, with the most common types being lung, renal, and melanoma. Evidence for donor origin of transmitted cancer is classified as proven, probable, possible, unlikely, or intervention taken without documented transmission, where genotyping provides the most substantial evidence. Given that our patient had a negative mammogram with no primary breast malignancy, the metastatic breast cancer probably originated from the transplanted liver. We have not yet seen a case of donor-transmitted metastatic breast cancer in a SOTR.
Disclosures:
Smriti Kochhar, DO1, Amee Pansuriya, DO1, Curtis McInnis, DO1, Fnu Anamika, MBBS2, Rohit Jain, MD1. P4748 - Metastatic Breast Cancer in a Liver Transplant Patient Originating From the Cadaver Donor, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2Delhi, Hershey, PA
Introduction: There is a 0.4% incidence of new post-transplant solid tumors in the United States. Malignancies in solid organ transplant recipients (SOTR) are concerning because these patients typically have a poor prognosis compared to the general population. Living donor screening involves a comprehensive review of the donor's medical history and physical examination, while deceased donor screening also involves testing for tumor markers. However, there is no universal protocol for cancer screening for solid organ transplants, and a few cases of cancer in SOTR have been reported. We present a case of a 58-year-old female who developed metastatic breast cancer from a transplanted donor liver.
Case Description/Methods: A 58-year-old female with a past medical history of cryptogenic cirrhosis status post orthotopic liver transplant one year ago (from a deceased breast cancer patient) on immunosuppression with tacrolimus and prednisone came to the hospital with abdominal and back pain. A CT abdomen showed new onset, diffuse hepatic hypodense lesions in the upper lobe, and a transjugular needle biopsy of the liver showed poorly differentiated carcinoma with necrosis involving the liver parenchyma, favoring metastatic breast carcinoma. Immunohistochemistry showed ER negative, PR-negative, and HER2 positive cells, and the tumor was also positive for panCK, CK7, MOC-31, GATA3, BRST-2 however, additional work-up with a mammogram ruled out primary malignancy. The bone scan showed mild focal uptake in the right scapula, with a brain MRI showing osseous metastasis within the right C1 lateral mass, C2 body, and left calvarium with no evidence of any intracranial metastatic disease. Systemic therapy with carboplatin/paclitaxel was initiated due to potential visceral crisis.
Discussion: Post transplantation, four types of cancers may occur: recurrent, donor-transmitted, donor-derived, and de novo. The rate of donor-transmitted cancers is less than 0.1%, with the most common types being lung, renal, and melanoma. Evidence for donor origin of transmitted cancer is classified as proven, probable, possible, unlikely, or intervention taken without documented transmission, where genotyping provides the most substantial evidence. Given that our patient had a negative mammogram with no primary breast malignancy, the metastatic breast cancer probably originated from the transplanted liver. We have not yet seen a case of donor-transmitted metastatic breast cancer in a SOTR.
Disclosures:
Smriti Kochhar indicated no relevant financial relationships.
Amee Pansuriya indicated no relevant financial relationships.
Curtis McInnis indicated no relevant financial relationships.
Fnu Anamika indicated no relevant financial relationships.
Rohit Jain indicated no relevant financial relationships.
Smriti Kochhar, DO1, Amee Pansuriya, DO1, Curtis McInnis, DO1, Fnu Anamika, MBBS2, Rohit Jain, MD1. P4748 - Metastatic Breast Cancer in a Liver Transplant Patient Originating From the Cadaver Donor, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
