Tuesday Poster Session
Category: Liver
P4751 - Endotipsitis: An Underdiagnosed Complication of Transjugular Intrahepatic Portosystemic Shunt Presenting as Septic Pulmonary Emboli
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AT
Asiya Tafader, MBBS
Virginia Commonwealth University Health System
Richmond, VA
Presenting Author(s)
Asiya Tafader, MBBS1, Spencer Harris, MD, PhD1, Scott Matherly, MD2
1Virginia Commonwealth University Health System, Richmond, VA; 2Virginia Commonwealth University, Richmond, VA
Introduction: Endotipsitis is a rare, life-threatening and seldom reported complication of Transjugular Intrahepatic Portosystemic Shunt (TIPS). We present a patient with endotipsitis and recurrent bacteremia complicated with septic embolic phenomena. Clinical practice guidelines are in dire need for this emerging nosocomial prosthetic-related infectious disease with a devastating mortality rate of 32%.
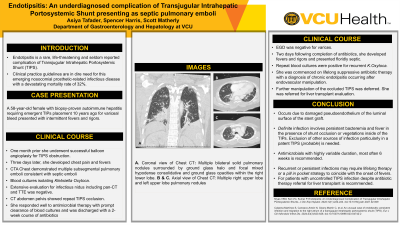
Case Description/Methods: A 58-year-old female with biopsy-proven autoimmune hepatitis requiring emergent TIPs placement 10 years ago for variceal bleed presented with intermittent fevers and rigors. One month prior she underwent successful balloon angioplasty for TIPS obstruction. Three days later, she developed chest pain and fevers with CTA Chest demonstrating multiple subsegmental pulmonary emboli and blood cultures isolating Klebsiella Oxytoca. Extensive evaluation for infectious nidus including pan-CT and TTE was negative. CT abdomen pelvis showed repeat TIPS occlusion. She responded well to antimicrobial therapy with prompt clearance of blood cultures and was discharged with a 2-week course of antibiotics. EGD was negative for varices. Two days following completion of antibiotics, she developed fevers and rigors and presented floridly septic. Repeat blood cultures were positive for recurrent K.Oxytoca.
She was commenced on lifelong suppressive antibiotic therapy with a diagnosis of chronic endotipsitis occurring after endovascular manipulation. Further manipulation of the occluded TIPS was deferred and she was referred for liver transplant evaluation.
Discussion: Endotipsitis is thought to occur due to damaged pseudoendothelium of the luminal surface of the stent with only approximately 70 cases reported. The definition is debated; definite clinical infection involves persistent bacteremia and fever in the presence of shunt occlusion or vegetations inside of the TIPs. The mainstay of treatment is antimicrobials with highly variable durations and most often, 6 weeks is recommended. Recurrent or persistent infections may require lifelong therapy and referral for liver transplant is recommended in uncontrolled infection. Little is known due to limited literature, risk factors include male gender and the etiology of cirrhosis and indication for TIPS does not seem to play a role.
The hurdles to diagnosis pivot around non-specific presentations and lack of awareness thus necessitating a high clinical suspicion in a patient with TIPS presenting with bacteremia.
Disclosures:
Asiya Tafader, MBBS1, Spencer Harris, MD, PhD1, Scott Matherly, MD2. P4751 - Endotipsitis: An Underdiagnosed Complication of Transjugular Intrahepatic Portosystemic Shunt Presenting as Septic Pulmonary Emboli, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Virginia Commonwealth University Health System, Richmond, VA; 2Virginia Commonwealth University, Richmond, VA
Introduction: Endotipsitis is a rare, life-threatening and seldom reported complication of Transjugular Intrahepatic Portosystemic Shunt (TIPS). We present a patient with endotipsitis and recurrent bacteremia complicated with septic embolic phenomena. Clinical practice guidelines are in dire need for this emerging nosocomial prosthetic-related infectious disease with a devastating mortality rate of 32%.
Case Description/Methods: A 58-year-old female with biopsy-proven autoimmune hepatitis requiring emergent TIPs placement 10 years ago for variceal bleed presented with intermittent fevers and rigors. One month prior she underwent successful balloon angioplasty for TIPS obstruction. Three days later, she developed chest pain and fevers with CTA Chest demonstrating multiple subsegmental pulmonary emboli and blood cultures isolating Klebsiella Oxytoca. Extensive evaluation for infectious nidus including pan-CT and TTE was negative. CT abdomen pelvis showed repeat TIPS occlusion. She responded well to antimicrobial therapy with prompt clearance of blood cultures and was discharged with a 2-week course of antibiotics. EGD was negative for varices. Two days following completion of antibiotics, she developed fevers and rigors and presented floridly septic. Repeat blood cultures were positive for recurrent K.Oxytoca.
She was commenced on lifelong suppressive antibiotic therapy with a diagnosis of chronic endotipsitis occurring after endovascular manipulation. Further manipulation of the occluded TIPS was deferred and she was referred for liver transplant evaluation.
Discussion: Endotipsitis is thought to occur due to damaged pseudoendothelium of the luminal surface of the stent with only approximately 70 cases reported. The definition is debated; definite clinical infection involves persistent bacteremia and fever in the presence of shunt occlusion or vegetations inside of the TIPs. The mainstay of treatment is antimicrobials with highly variable durations and most often, 6 weeks is recommended. Recurrent or persistent infections may require lifelong therapy and referral for liver transplant is recommended in uncontrolled infection. Little is known due to limited literature, risk factors include male gender and the etiology of cirrhosis and indication for TIPS does not seem to play a role.
The hurdles to diagnosis pivot around non-specific presentations and lack of awareness thus necessitating a high clinical suspicion in a patient with TIPS presenting with bacteremia.
Disclosures:
Asiya Tafader indicated no relevant financial relationships.
Spencer Harris indicated no relevant financial relationships.
Scott Matherly indicated no relevant financial relationships.
Asiya Tafader, MBBS1, Spencer Harris, MD, PhD1, Scott Matherly, MD2. P4751 - Endotipsitis: An Underdiagnosed Complication of Transjugular Intrahepatic Portosystemic Shunt Presenting as Septic Pulmonary Emboli, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
