Tuesday Poster Session
Category: Liver
P4753 - A Rare Case of Olanzapine-Induced Liver Injury Due to DRESS Syndrome
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Krishna Patel, MD
Emory University School of Medicine
Atlanta, GA
Presenting Author(s)
Krishna Patel, MD, Rishi Das, MD, MPH, Elnaz Jafarimehr, MD, Patrick Arraj, MD, Alyssa Krasinskas, MD
Emory University School of Medicine, Atlanta, GA
Introduction: Amongst psychotropic medications, anti-epileptics are more commonly implicated as causes of drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome. However, anti-psychotics such as olanzapine can also cause DRESS, though it is incredibly rare. In 2016, the FDA issued a blackbox warning for olanzapine for its association with DRESS based on 23 reported cases since 1996 in the adverse event reporting system. Given the variety in patient presentation, DRESS is often difficult to diagnosis and a missed diagnosis leads to poor patient outcomes. The identification of DRESS due to olanzapine use can be confounded by polypharmacy and overlapping clinical presentation with select hematological conditions.
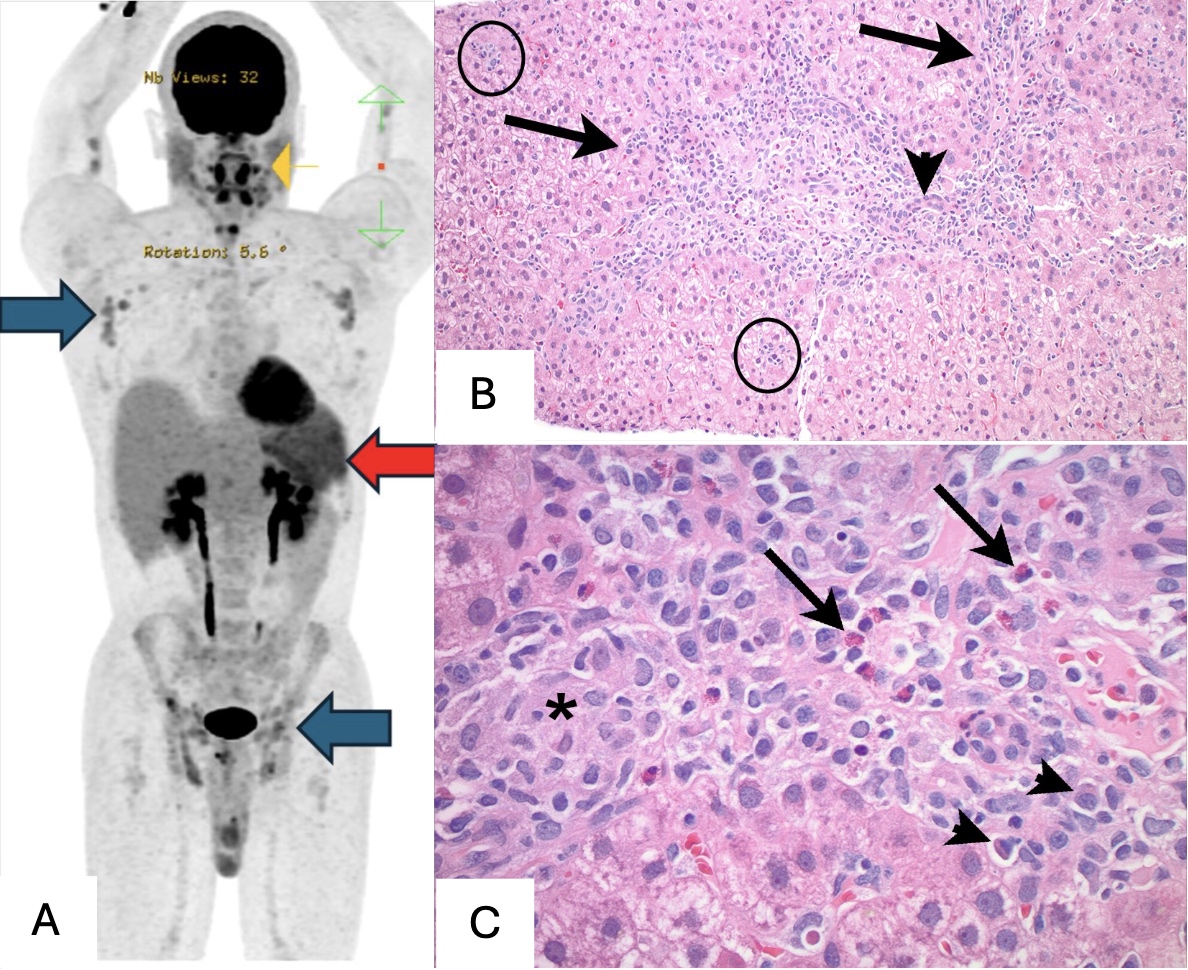
Case Description/Methods: A 25-year-old male with a history of HIV and substance-induced psychosis presented from a prison facility with fevers, bony pain, facial edema, and a diffuse maculopapular rash. He started olanzapine for psychosis 2 months prior to presentation. Given his history of HIV and incarceration, a thorough autoimmune and infectious workup was done and non-revealing. By day 7 of his hospitalization, the patient developed lymphocytic leukocytosis with eosinophilia, severe thrombocytopenia, and acute hepatocellular liver injury. A whole-body PET scan was revealing for multistation lymphadenopathy (LAD) and splenomegaly. On day 13, the patient underwent an excisional lymph node biopsy, which was negative for malignant lymphoma. Ultimately, a liver biopsy was done which showed mixed portal and lobular inflammation with scattered apoptotic bodies and interface activity, consistent with an active hepatitis, favoring drug-induced liver injury and supporting the clinical impression of DRESS. By the time the liver biopsy was done, olanzapine was stopped, and the patient’s symptoms and LFTs were improving without steroid therapy.
Discussion: Olanzapine use is associated with transient, self-resolving transaminitis in 10-50% of patients, however, an immunoallergic reaction involving fever, rash, and acute hepatitis is uncommon and rare. Although this patient had a rash and eosinophilia, his diagnosis was delayed due to suspicion for lymphoproliferative disorder given his chronic immunosuppression history with HIV, leukocytosis, LAD, and splenomegaly. A challenge with DRESS diagnosis is the latency period between drug initiation and symptom onset. DRESS syndrome can be fatal and prompt diagnosis is important for discontinuing the offending drug to prevent further liver injury.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Krishna Patel, MD, Rishi Das, MD, MPH, Elnaz Jafarimehr, MD, Patrick Arraj, MD, Alyssa Krasinskas, MD. P4753 - A Rare Case of Olanzapine-Induced Liver Injury Due to DRESS Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Emory University School of Medicine, Atlanta, GA
Introduction: Amongst psychotropic medications, anti-epileptics are more commonly implicated as causes of drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome. However, anti-psychotics such as olanzapine can also cause DRESS, though it is incredibly rare. In 2016, the FDA issued a blackbox warning for olanzapine for its association with DRESS based on 23 reported cases since 1996 in the adverse event reporting system. Given the variety in patient presentation, DRESS is often difficult to diagnosis and a missed diagnosis leads to poor patient outcomes. The identification of DRESS due to olanzapine use can be confounded by polypharmacy and overlapping clinical presentation with select hematological conditions.
Case Description/Methods: A 25-year-old male with a history of HIV and substance-induced psychosis presented from a prison facility with fevers, bony pain, facial edema, and a diffuse maculopapular rash. He started olanzapine for psychosis 2 months prior to presentation. Given his history of HIV and incarceration, a thorough autoimmune and infectious workup was done and non-revealing. By day 7 of his hospitalization, the patient developed lymphocytic leukocytosis with eosinophilia, severe thrombocytopenia, and acute hepatocellular liver injury. A whole-body PET scan was revealing for multistation lymphadenopathy (LAD) and splenomegaly. On day 13, the patient underwent an excisional lymph node biopsy, which was negative for malignant lymphoma. Ultimately, a liver biopsy was done which showed mixed portal and lobular inflammation with scattered apoptotic bodies and interface activity, consistent with an active hepatitis, favoring drug-induced liver injury and supporting the clinical impression of DRESS. By the time the liver biopsy was done, olanzapine was stopped, and the patient’s symptoms and LFTs were improving without steroid therapy.
Discussion: Olanzapine use is associated with transient, self-resolving transaminitis in 10-50% of patients, however, an immunoallergic reaction involving fever, rash, and acute hepatitis is uncommon and rare. Although this patient had a rash and eosinophilia, his diagnosis was delayed due to suspicion for lymphoproliferative disorder given his chronic immunosuppression history with HIV, leukocytosis, LAD, and splenomegaly. A challenge with DRESS diagnosis is the latency period between drug initiation and symptom onset. DRESS syndrome can be fatal and prompt diagnosis is important for discontinuing the offending drug to prevent further liver injury.
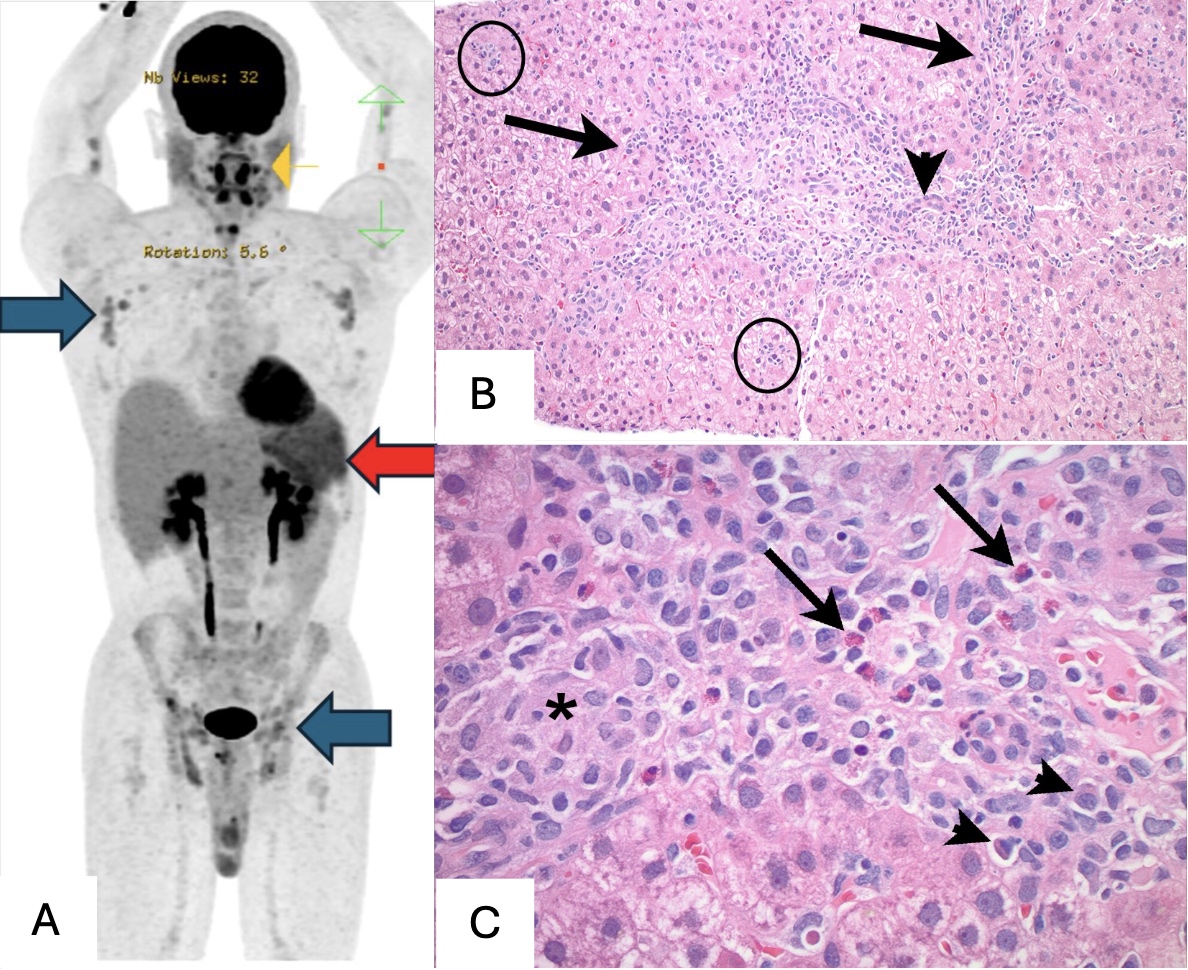
Figure: A: PET scan with nonspecific, diffuse axillary and inguinal lymphadenopathy (blue arrows) and splenomegaly (red arrow). B: Histopathology showing a portal tract expanded by mixed inflammation with interface activity (arrows) and inflammation in the lobules (circled); a bile duct is uninvolved (arrowhead) (under H&E stain, at magnification 100x). C: Histopathology of a portal tract with a mixture of histiocytes (*), eosinophils (arrows), plasma cells (arrowheads) and scattered lymphocytes (under H&E stain, at magnification 100x).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Krishna Patel indicated no relevant financial relationships.
Rishi Das indicated no relevant financial relationships.
Elnaz Jafarimehr indicated no relevant financial relationships.
Patrick Arraj indicated no relevant financial relationships.
Alyssa Krasinskas indicated no relevant financial relationships.
Krishna Patel, MD, Rishi Das, MD, MPH, Elnaz Jafarimehr, MD, Patrick Arraj, MD, Alyssa Krasinskas, MD. P4753 - A Rare Case of Olanzapine-Induced Liver Injury Due to DRESS Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
