Tuesday Poster Session
Category: Liver
P4756 - Rescue PAATO/CAATO for Recurrent Peristomal Variceal Bleeding Secondary to Hepatic Metastases Causing Portal Hypertension
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Naren Nallapeta, MD
University at Buffalo
Buffalo, NY
Presenting Author(s)
Award: Presidential Poster Award
Naren Nallapeta, MD1, Clive J. Miranda, DO, MSc2, Alexander M. Carlson, DO1, Ali A. Aijaz, DO1, Nariman Hossein-Javaheri, DO1, Ikjot Singh, MD1, Courtney Dennis, MD3, Srushti Sahukar, MBBS4, Thomas Mahl, MD1
1University at Buffalo, Buffalo, NY; 2CHI Health Creighton University Medical Center, Omaha, NE; 3University of Buffalo, Buffalo, NY; 4SUNY Upstate Medical University, North Billerica, MA
Introduction: Ectopic varices account to about 5% of all variceal bleeding with a mortality rate of 3-4%.
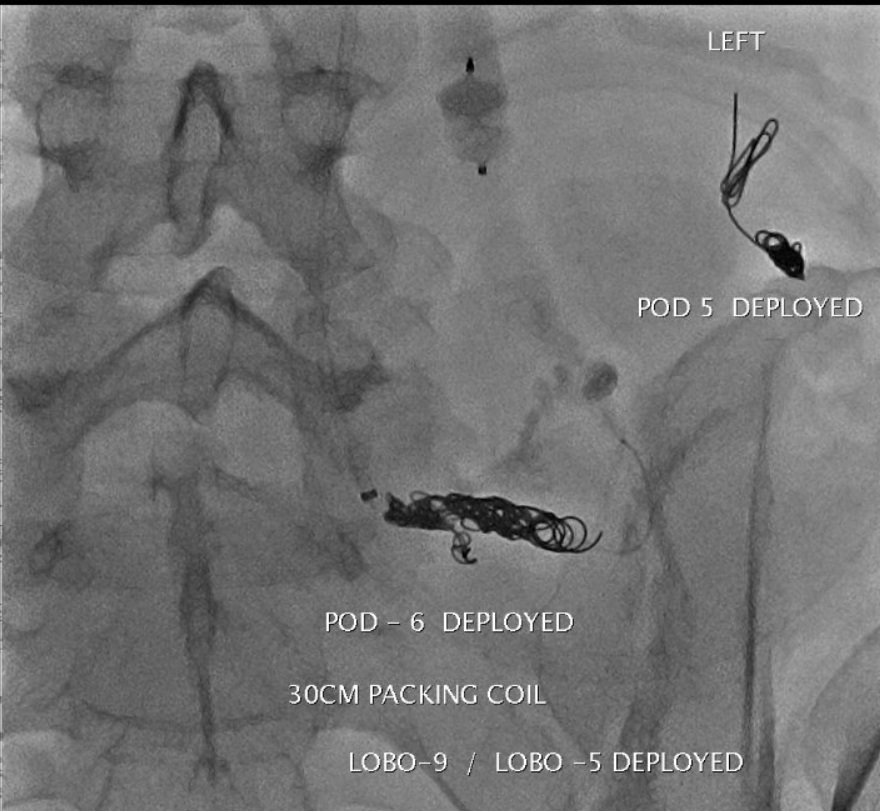
Case Description/Methods: 43 year-old male presented to the emergency room (ER) with diarrhea for 2 months & intermittent bleeding. Labs significant for hemoglobin 2.9 g/dl, MCV 71.8 fl. Colonoscopy showed a partially obstructing fungating, friable mass in the sigmoid colon. Biopsies showed adenocarcinoma. CT abdomen showed innumerable lesions in the liver and biopsies consistent with adenocarcinoma. He was treated with chemotherapy but lost to follow up. He presented to the emergency room about 5 months after with a large bowel obstruction and a colostomy was performed. Two months later imaging showing progression of hepatic metastatic disease, retroperitoneal and pulmonary metastases. He then presented to the ER with melena through the colostomy. Upper endoscopy and colonoscopy through the ostomy site both of which were negative for any active signs of bleeding or any etiology identified for bleeding. He had pancytopenia. Ultrasound of the liver noted patent portal vein and hepatopetal flow. CT showing sequalae of portal hypertension including splenomegaly, ascites with gastroesophageal and large ectopic peristomal varices. Bleeding recurred and despite careful endoscopic inspection, varices were not visible near the ostomy. Given clinical concern for peristomal variceal bleeding, he had an intervention radiology (IR) guided percutaneous plug and coil assisted antegrade transhepatic obliteration (PAATO and CAATO) of 3 different feeding vessels that was successful in preventing further bleeding. After discharge, he was continued on chemotherapy. No bleeding noted since.
Discussion: We present an interesting case of peristomal varices secondary to portal hypertension from colon cancer metastases to the liver requiring IR guided embolization. Patient had no known liver disease prior to the metastatic colon cancer and negative endoscopies. Using IR guided embolization as a rescue therapy prevented further morbidity. Transjugular intrahepatic portosystemic shunt (TIPS) although a rescue therapy was not on option given patient’s poor liver function.
Multiple modalities for treatment of bleeding have been described including TIPS, percutaneous transhepatic route, percutaneous trans-splenic approach, balloon-occluded retrograde transvenous occlusion (BRTO), direct percutaneous puncture with subsequent embolization, endoscopic ultrasound (EUS) guided coil embolization have been described to control bleeding.
Disclosures:
Naren Nallapeta, MD1, Clive J. Miranda, DO, MSc2, Alexander M. Carlson, DO1, Ali A. Aijaz, DO1, Nariman Hossein-Javaheri, DO1, Ikjot Singh, MD1, Courtney Dennis, MD3, Srushti Sahukar, MBBS4, Thomas Mahl, MD1. P4756 - Rescue PAATO/CAATO for Recurrent Peristomal Variceal Bleeding Secondary to Hepatic Metastases Causing Portal Hypertension, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Naren Nallapeta, MD1, Clive J. Miranda, DO, MSc2, Alexander M. Carlson, DO1, Ali A. Aijaz, DO1, Nariman Hossein-Javaheri, DO1, Ikjot Singh, MD1, Courtney Dennis, MD3, Srushti Sahukar, MBBS4, Thomas Mahl, MD1
1University at Buffalo, Buffalo, NY; 2CHI Health Creighton University Medical Center, Omaha, NE; 3University of Buffalo, Buffalo, NY; 4SUNY Upstate Medical University, North Billerica, MA
Introduction: Ectopic varices account to about 5% of all variceal bleeding with a mortality rate of 3-4%.
Case Description/Methods: 43 year-old male presented to the emergency room (ER) with diarrhea for 2 months & intermittent bleeding. Labs significant for hemoglobin 2.9 g/dl, MCV 71.8 fl. Colonoscopy showed a partially obstructing fungating, friable mass in the sigmoid colon. Biopsies showed adenocarcinoma. CT abdomen showed innumerable lesions in the liver and biopsies consistent with adenocarcinoma. He was treated with chemotherapy but lost to follow up. He presented to the emergency room about 5 months after with a large bowel obstruction and a colostomy was performed. Two months later imaging showing progression of hepatic metastatic disease, retroperitoneal and pulmonary metastases. He then presented to the ER with melena through the colostomy. Upper endoscopy and colonoscopy through the ostomy site both of which were negative for any active signs of bleeding or any etiology identified for bleeding. He had pancytopenia. Ultrasound of the liver noted patent portal vein and hepatopetal flow. CT showing sequalae of portal hypertension including splenomegaly, ascites with gastroesophageal and large ectopic peristomal varices. Bleeding recurred and despite careful endoscopic inspection, varices were not visible near the ostomy. Given clinical concern for peristomal variceal bleeding, he had an intervention radiology (IR) guided percutaneous plug and coil assisted antegrade transhepatic obliteration (PAATO and CAATO) of 3 different feeding vessels that was successful in preventing further bleeding. After discharge, he was continued on chemotherapy. No bleeding noted since.
Discussion: We present an interesting case of peristomal varices secondary to portal hypertension from colon cancer metastases to the liver requiring IR guided embolization. Patient had no known liver disease prior to the metastatic colon cancer and negative endoscopies. Using IR guided embolization as a rescue therapy prevented further morbidity. Transjugular intrahepatic portosystemic shunt (TIPS) although a rescue therapy was not on option given patient’s poor liver function.
Multiple modalities for treatment of bleeding have been described including TIPS, percutaneous transhepatic route, percutaneous trans-splenic approach, balloon-occluded retrograde transvenous occlusion (BRTO), direct percutaneous puncture with subsequent embolization, endoscopic ultrasound (EUS) guided coil embolization have been described to control bleeding.
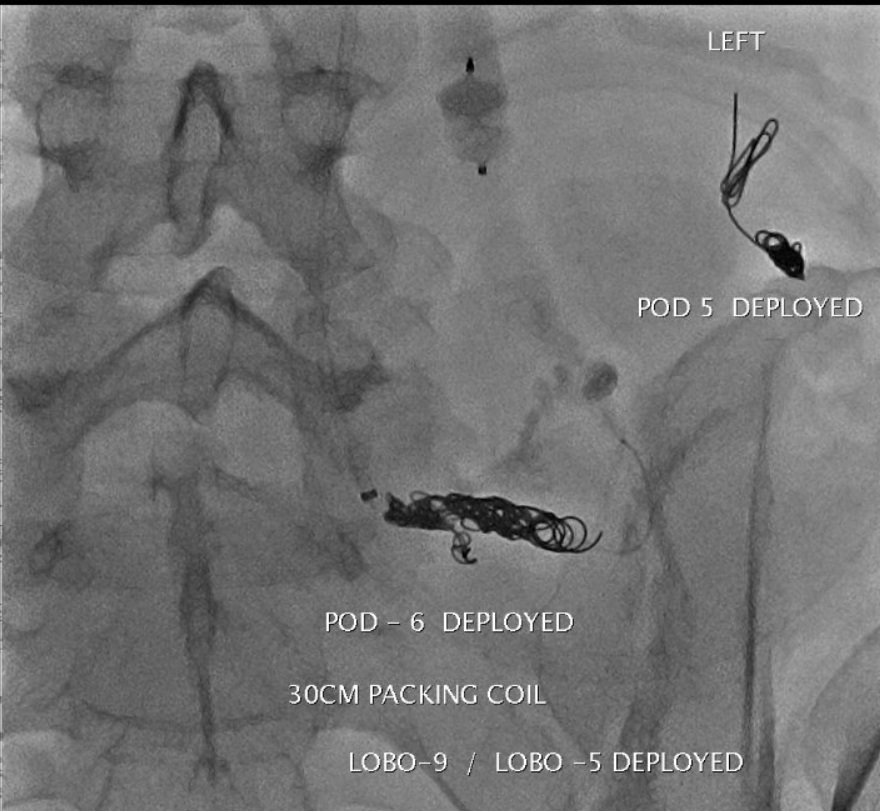
Figure: Angiography pictures post coils
Disclosures:
Naren Nallapeta indicated no relevant financial relationships.
Clive Miranda indicated no relevant financial relationships.
Alexander Carlson indicated no relevant financial relationships.
Ali Aijaz indicated no relevant financial relationships.
Nariman Hossein-Javaheri indicated no relevant financial relationships.
Ikjot Singh indicated no relevant financial relationships.
Courtney Dennis indicated no relevant financial relationships.
Srushti Sahukar indicated no relevant financial relationships.
Thomas Mahl indicated no relevant financial relationships.
Naren Nallapeta, MD1, Clive J. Miranda, DO, MSc2, Alexander M. Carlson, DO1, Ali A. Aijaz, DO1, Nariman Hossein-Javaheri, DO1, Ikjot Singh, MD1, Courtney Dennis, MD3, Srushti Sahukar, MBBS4, Thomas Mahl, MD1. P4756 - Rescue PAATO/CAATO for Recurrent Peristomal Variceal Bleeding Secondary to Hepatic Metastases Causing Portal Hypertension, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

