Tuesday Poster Session
Category: Liver
P4760 - An Unusual Case of Bleeding Varices: Hepatic Schistosomiasis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jordan Carty, MD
Albert Einstein Medical Center
Philadelphia, PA
Presenting Author(s)
Jordan Carty, MD1, Kevin Robinson, MD1, Jessica Genkil, DO2, Simone A. Jarrett, MBBS1, Zurab Azmaiparashvili, MD, MSc3, Kevin Lo, MD4, Maria Lagarde Mussa, MD5
1Albert Einstein Medical Center, Philadelphia, PA; 2Jefferson Einstein, Huntingdon Valley, PA; 3Jefferson Einstein Hospital, Philadelphia, PA; 4Brigham and Women's Hospital, Boston, MA; 5Einstein Medical Center, Philadelphia, PA
Introduction: Schistosomiasis an uncommon cause of bleeding esophageal varices within the western region. We report a case of schistosomiasis leading to bleeding esophageal varices.
Case Description/Methods: A 48-year-old Malian male with history of hypertension, hyperlipidemia and social alcohol use, presented with acute onset hematemesis. He was recently hospitalized with upper gastrointestinal bleeding attributed to esophageal varices for which he underwent endoscopic ligation. A computed tomography scan of the abdomen and pelvis showed normal appearance of the liver and spleen, with no signs of liver cirrhosis. At that time, he was discharged on carvedilol for secondary prevention of esophageal varices.
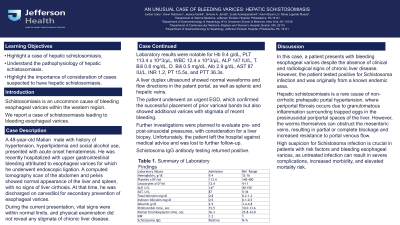
During the current presentation, vital signs were within normal limits, and physical examination did not reveal any stigmata of chronic liver disease. Laboratory results were notable for Hb 9.4 g/dL, PLT 113.4 x 10^3/µL, WBC 12.4 x 10^3/µL, ALP 147 IU/L, T. Bili 0.8 mg/dL, I. Bili 0.5 mg/dL, Alb 2.9 g/dL, AST 87 IU/L, INR 1.2, PT 15.5s, and PTT 36.3s. A liver duplex ultrasound showed normal waveforms and flow directions in the patent portal veins, splenic veins, and hepatic veins. Patient underwent an urgent EGD which confirmed the successful placement of prior variceal bands, but also showed additional varices with stigmata of recent bleeding. Further investigations were planned to evaluate pre- and post-sinusoidal pressures, with consideration for a liver biopsy. Unfortunately, the patient left the hospital against medical advice, and he was lost to further follow-up. Schistosoma IgG antibody testing returned positive.
Discussion: In this case, a patient presents with bleeding esophageal varices, despite the absence of clinical and radiological signs of chronic liver disease. However, the patient tested positive for Schistosoma infection and was originally from a known endemic area. Hepatic schistosomiasis is a rare cause of non-cirrhotic prehepatic portal hypertension, where periportal fibrosis occurs due to granulomatous inflammation surrounding trapped eggs in the presinusoidal periportal spaces of the liver. However, the worms themselves can cause obstruction in the mesenteric veins, resulting in partial or complete blockage and increased resistance to portal venous flow. High suspicion for Schistosoma infection is crucial in patients with risk factors and bleeding esophageal varices, as untreated infection can result in severe complications, increased morbidity, and elevated mortality risk.
Disclosures:
Jordan Carty, MD1, Kevin Robinson, MD1, Jessica Genkil, DO2, Simone A. Jarrett, MBBS1, Zurab Azmaiparashvili, MD, MSc3, Kevin Lo, MD4, Maria Lagarde Mussa, MD5. P4760 - An Unusual Case of Bleeding Varices: Hepatic Schistosomiasis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Albert Einstein Medical Center, Philadelphia, PA; 2Jefferson Einstein, Huntingdon Valley, PA; 3Jefferson Einstein Hospital, Philadelphia, PA; 4Brigham and Women's Hospital, Boston, MA; 5Einstein Medical Center, Philadelphia, PA
Introduction: Schistosomiasis an uncommon cause of bleeding esophageal varices within the western region. We report a case of schistosomiasis leading to bleeding esophageal varices.
Case Description/Methods: A 48-year-old Malian male with history of hypertension, hyperlipidemia and social alcohol use, presented with acute onset hematemesis. He was recently hospitalized with upper gastrointestinal bleeding attributed to esophageal varices for which he underwent endoscopic ligation. A computed tomography scan of the abdomen and pelvis showed normal appearance of the liver and spleen, with no signs of liver cirrhosis. At that time, he was discharged on carvedilol for secondary prevention of esophageal varices.
During the current presentation, vital signs were within normal limits, and physical examination did not reveal any stigmata of chronic liver disease. Laboratory results were notable for Hb 9.4 g/dL, PLT 113.4 x 10^3/µL, WBC 12.4 x 10^3/µL, ALP 147 IU/L, T. Bili 0.8 mg/dL, I. Bili 0.5 mg/dL, Alb 2.9 g/dL, AST 87 IU/L, INR 1.2, PT 15.5s, and PTT 36.3s. A liver duplex ultrasound showed normal waveforms and flow directions in the patent portal veins, splenic veins, and hepatic veins. Patient underwent an urgent EGD which confirmed the successful placement of prior variceal bands, but also showed additional varices with stigmata of recent bleeding. Further investigations were planned to evaluate pre- and post-sinusoidal pressures, with consideration for a liver biopsy. Unfortunately, the patient left the hospital against medical advice, and he was lost to further follow-up. Schistosoma IgG antibody testing returned positive.
Discussion: In this case, a patient presents with bleeding esophageal varices, despite the absence of clinical and radiological signs of chronic liver disease. However, the patient tested positive for Schistosoma infection and was originally from a known endemic area. Hepatic schistosomiasis is a rare cause of non-cirrhotic prehepatic portal hypertension, where periportal fibrosis occurs due to granulomatous inflammation surrounding trapped eggs in the presinusoidal periportal spaces of the liver. However, the worms themselves can cause obstruction in the mesenteric veins, resulting in partial or complete blockage and increased resistance to portal venous flow. High suspicion for Schistosoma infection is crucial in patients with risk factors and bleeding esophageal varices, as untreated infection can result in severe complications, increased morbidity, and elevated mortality risk.
Disclosures:
Jordan Carty indicated no relevant financial relationships.
Kevin Robinson indicated no relevant financial relationships.
Jessica Genkil indicated no relevant financial relationships.
Simone Jarrett indicated no relevant financial relationships.
Zurab Azmaiparashvili indicated no relevant financial relationships.
Kevin Lo indicated no relevant financial relationships.
Maria Lagarde Mussa indicated no relevant financial relationships.
Jordan Carty, MD1, Kevin Robinson, MD1, Jessica Genkil, DO2, Simone A. Jarrett, MBBS1, Zurab Azmaiparashvili, MD, MSc3, Kevin Lo, MD4, Maria Lagarde Mussa, MD5. P4760 - An Unusual Case of Bleeding Varices: Hepatic Schistosomiasis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
