Tuesday Poster Session
Category: Liver
P4763 - Unmasking the Deceiver: Autoimmune Hepatitis Disguised as Lymphoma
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Ahamed Khalyfa, DO
University of Iowa
Iowa City, IA
Presenting Author(s)
Ahamed Khalyfa, DO1, Antonio J. Sanchez, MD2, Yasameen Muzahim, MD2
1University of Iowa, Iowa City, IA; 2University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: Autoimmune hepatitis (AIH) is an immune- mediated inflammatory liver disease that can progress to advanced hepatic fibrosis, cirrhosis and liver failure which makes early diagnosis crucial yet challenging as it lacks signature diagnostic features, and sometimes it manifests in a rare presentation like our patient’s.
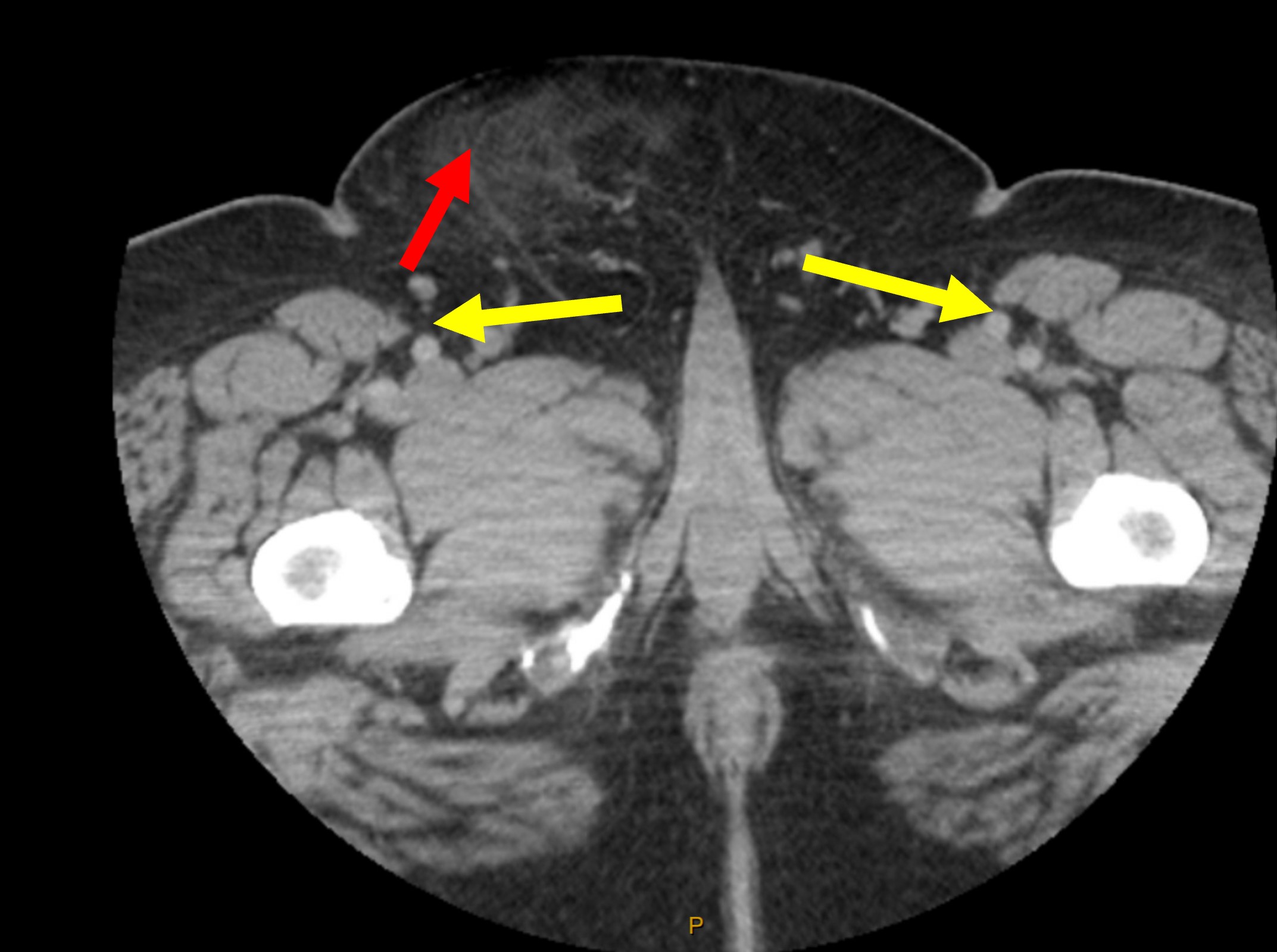
Case Description/Methods: We present the case of a 54-year-old man who was admitted to the hospital with new onset jaundice, worsening fatigue, right lower abdominal quadrant and right groin fullness. He denied fever, or unintentional weight loss. Initial laboratory tests showed total bilirubin 8.5 mg/dL, direct bilirubin 5.8 mg/dL, AST 456 IU/L, ALT 228 IU/L, and ALP 133 IU/L. Chronic liver disease workup was unremarkable except for positive anti-smooth muscle antibodies and serum IgG 3962 mg/dL. CT chest, abdomen and pelvis with contrast showed hepatosplenomegaly with multiple enlarged upper abdominal and retroperitoneal lymph nodes, including periportal, portocaval, and paraaortic lymph nodes with pleuropulmonary nodules and an infiltrative process of the right lower quadrant (Fig.1). The pathology result of a biopsy of the abdominal mass was consistent with fat necrosis. A liver biopsy revealed pan lobular inflammatory infiltration of predominantly plasma cells, lymphocytes, and histiocytes with hepatocyte necrosis suggestive of AIH. After a year of treatment with prednisone and azathioprine, blood test showed total bilirubin 0.6 mg/dL, AST 61 IU/L, ALT 52 IU/L. A repeat CT abdomen with contrast showed interval decrease of periportal, peripancreatic and retroperitoneal lymphadenopathy compared to prior exam (Fig.2). A repeat liver biopsy showed persistent lobular inflammation from AIH which was decreased from previous biopsy. An increase in his immunosuppressive therapy led to normalization of liver enzymes. A subsequent CT abdomen with contrast showed complete resolution of lymphadenopathy (Fig.3). 13 years after his initial presentation, the patient remains stable without AIH flares or liver disease progression.
Discussion: AIH can cause progressive liver injury, and early diagnosis significantly impacts the outcome. We have a unique presentation of AIH characterized by diffuse lymphadenopathy, initially concerning for lymphoma. The clinical outcome of our patient highlights the importance of recognizing the association of AIH with diffuse lymphadenopathy mimicking lymphoma, and it also emphasizes that adequate treatment of AIH leads to resolution of the lymphadenopathy.
Disclosures:
Ahamed Khalyfa, DO1, Antonio J. Sanchez, MD2, Yasameen Muzahim, MD2. P4763 - Unmasking the Deceiver: Autoimmune Hepatitis Disguised as Lymphoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Iowa, Iowa City, IA; 2University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: Autoimmune hepatitis (AIH) is an immune- mediated inflammatory liver disease that can progress to advanced hepatic fibrosis, cirrhosis and liver failure which makes early diagnosis crucial yet challenging as it lacks signature diagnostic features, and sometimes it manifests in a rare presentation like our patient’s.
Case Description/Methods: We present the case of a 54-year-old man who was admitted to the hospital with new onset jaundice, worsening fatigue, right lower abdominal quadrant and right groin fullness. He denied fever, or unintentional weight loss. Initial laboratory tests showed total bilirubin 8.5 mg/dL, direct bilirubin 5.8 mg/dL, AST 456 IU/L, ALT 228 IU/L, and ALP 133 IU/L. Chronic liver disease workup was unremarkable except for positive anti-smooth muscle antibodies and serum IgG 3962 mg/dL. CT chest, abdomen and pelvis with contrast showed hepatosplenomegaly with multiple enlarged upper abdominal and retroperitoneal lymph nodes, including periportal, portocaval, and paraaortic lymph nodes with pleuropulmonary nodules and an infiltrative process of the right lower quadrant (Fig.1). The pathology result of a biopsy of the abdominal mass was consistent with fat necrosis. A liver biopsy revealed pan lobular inflammatory infiltration of predominantly plasma cells, lymphocytes, and histiocytes with hepatocyte necrosis suggestive of AIH. After a year of treatment with prednisone and azathioprine, blood test showed total bilirubin 0.6 mg/dL, AST 61 IU/L, ALT 52 IU/L. A repeat CT abdomen with contrast showed interval decrease of periportal, peripancreatic and retroperitoneal lymphadenopathy compared to prior exam (Fig.2). A repeat liver biopsy showed persistent lobular inflammation from AIH which was decreased from previous biopsy. An increase in his immunosuppressive therapy led to normalization of liver enzymes. A subsequent CT abdomen with contrast showed complete resolution of lymphadenopathy (Fig.3). 13 years after his initial presentation, the patient remains stable without AIH flares or liver disease progression.
Discussion: AIH can cause progressive liver injury, and early diagnosis significantly impacts the outcome. We have a unique presentation of AIH characterized by diffuse lymphadenopathy, initially concerning for lymphoma. The clinical outcome of our patient highlights the importance of recognizing the association of AIH with diffuse lymphadenopathy mimicking lymphoma, and it also emphasizes that adequate treatment of AIH leads to resolution of the lymphadenopathy.
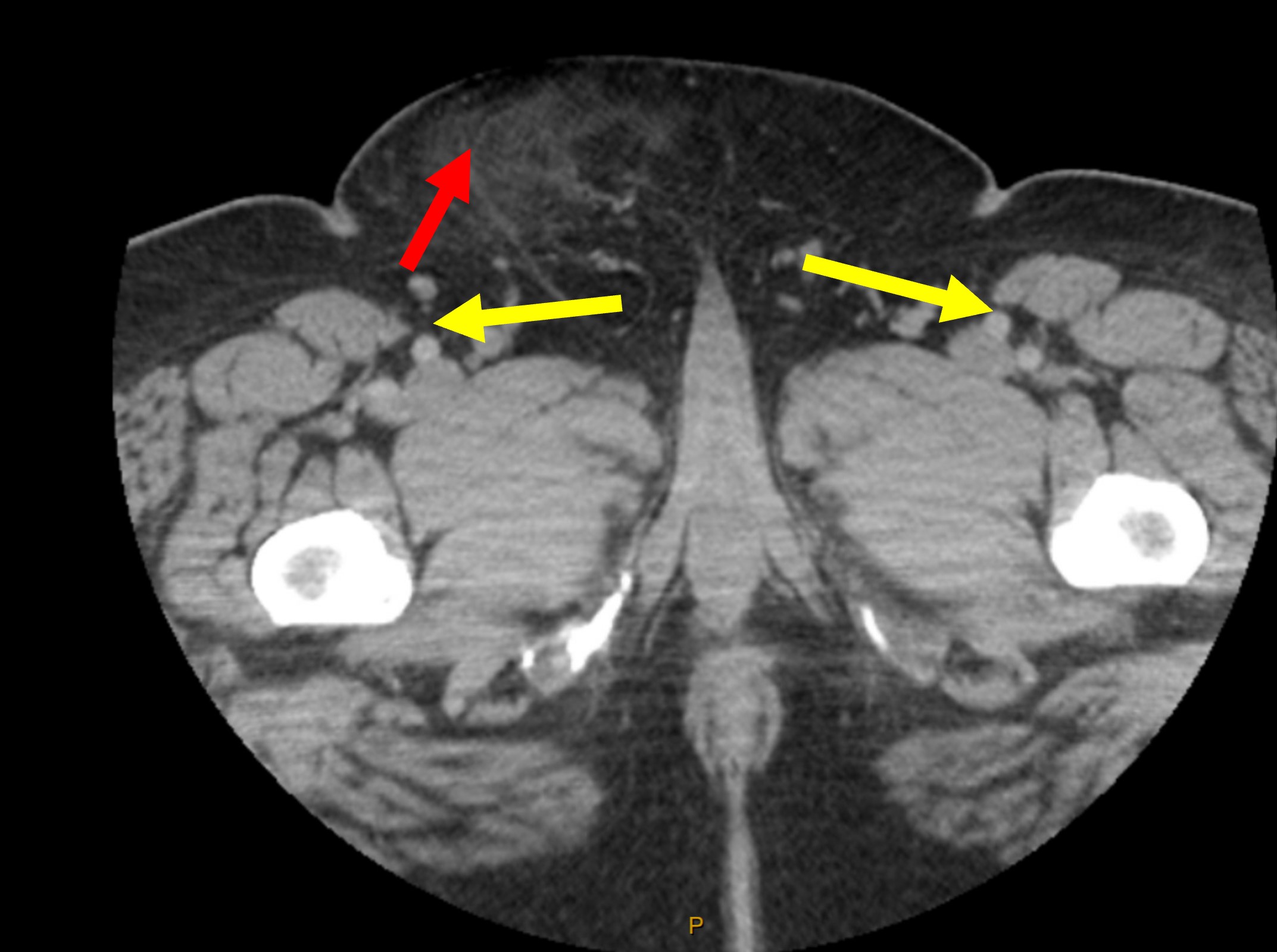
Figure: Initial CT scan showing RLQ enhancement concerning for infiltrative process (red arrow) with lymphadenopathy (yellow arrows)
Disclosures:
Ahamed Khalyfa indicated no relevant financial relationships.
Antonio Sanchez: Abbvie – Grant/Research Support. Boehringer-Ingelheim – Grant/Research Support. Gilead – Grant/Research Support. Inventiva – Grant/Research Support. Ipsen – Advisory Committee/Board Member. Merck – Grant/Research Support. Mirum Pharmaceuticals – Grant/Research Support. Takeda – Grant/Research Support.
Yasameen Muzahim indicated no relevant financial relationships.
Ahamed Khalyfa, DO1, Antonio J. Sanchez, MD2, Yasameen Muzahim, MD2. P4763 - Unmasking the Deceiver: Autoimmune Hepatitis Disguised as Lymphoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
