Tuesday Poster Session
Category: Liver
P4766 - Ascites as a Harbinger of Peritoneal and Hepatic Amyloidosis in AL Amyloidosis and Multiple Myeloma Intersection
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Zehra Naseem, MD
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Zehra Naseem, MD1, Arjun Chatterjee, MD1, Muyiwa Awoniyi, MD2, Sandra Mazzoni, MD1, Sobia Laique, MD1
1Cleveland Clinic, Cleveland, OH; 2Digestive Disease Institute, Cleveland Clinic, Cleveland, OH
Introduction: Amyloidosis disrupts organ function by depositing amyloid fibrils. The clinical presentation varies depending on the type of amyloid and its accumulation site. While gastrointestinal symptoms are frequently observed, hepatic and peritoneal amyloidosis accompanied by ascites is uncommon. Here, we report a rare case of worsening ascites due to co-existing hepatic and peritoneal amyloidosis in a patient with multisystemic AL amyloidosis and multiple myeloma, detailing our management approach.
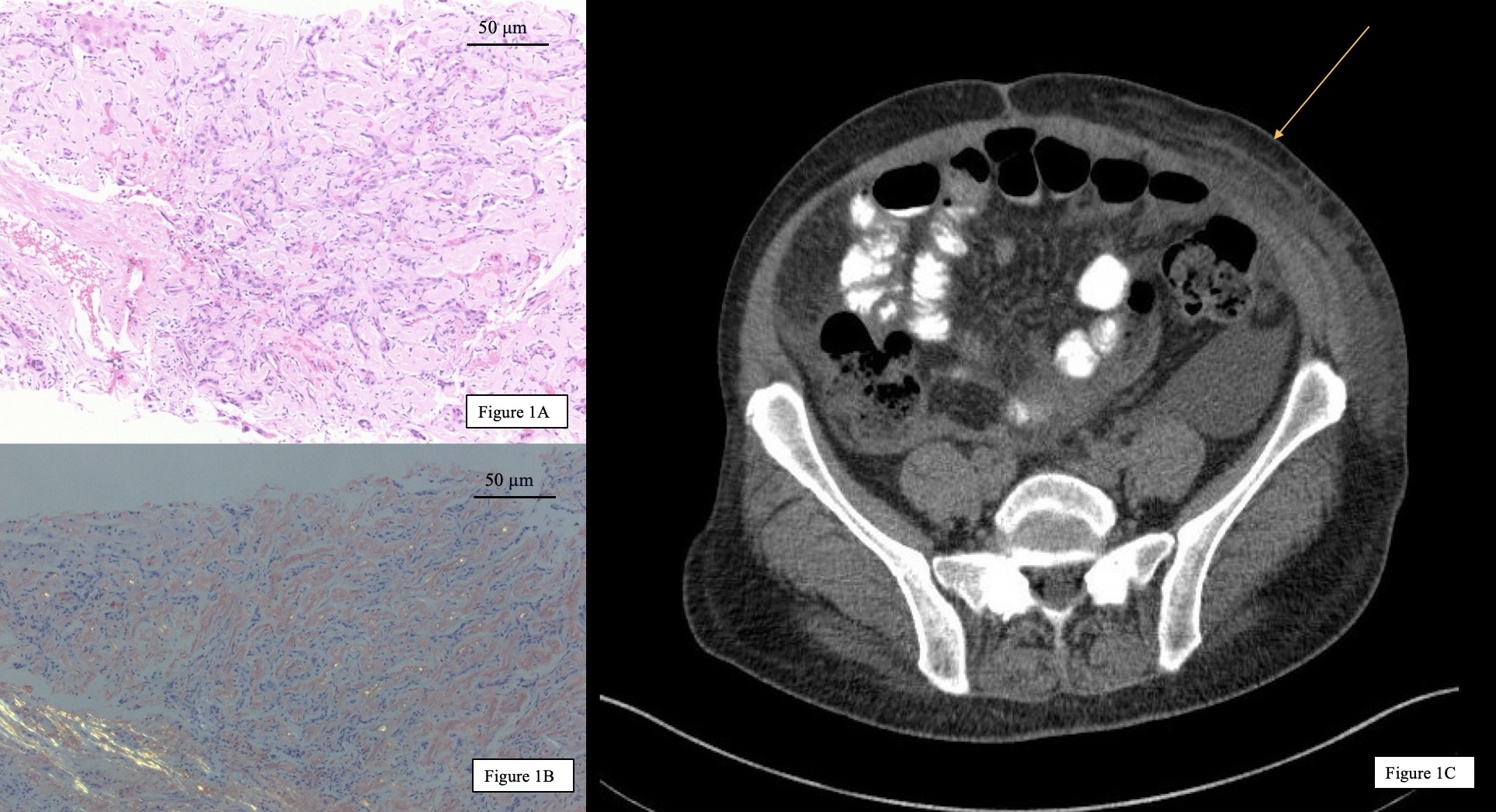
Case Description/Methods: A 53-year-old woman with multiple myeloma and biopsy-proven AL amyloidosis involving her liver (Figure 1A and 1B), heart, and bone marrow was hospitalized due to rapidly worsening ascites and shortness of breath. Despite six months of treatment with Daratumumab and CyBorD (as per the ANDROMEDA trial), supplemented by diuretics, her symptoms progressed, necessitating frequent paracentesis.
Chest X-rays ruled out pleural effusion, and no deterioration was observed in her cardiac, renal, or hepatic functions. Alkaline phosphatase levels remained chronically elevated at 900-1000 U/L, and the serum-ascites albumin gradient (SAAG) consistently exceeded 1.1 (Table 1), indicating portal hypertension. However, the hepatic venous pressure gradient (HVPG) was normal at 4, suggesting pre-sinusoidal congestion. An abdominal CT scan (Figure 1C) revealed omental and peritoneal fat stranding, consistent with amyloid infiltration.
The patient was discharged in stable condition with a treatment plan that included ongoing diuretics and scheduled paracentesis. She transitioned to a regimen of bortezomib, venetoclax, and daratumumab, which suppressed her light chain production, leading to improved ascites.
Discussion: Ascites in peritoneal amyloidosis is extremely rare, with only one reported case involving concurrent hepatic amyloidosis. Therefore, peritoneal involvement by amyloidosis should be considered in an ascitic patient with relatively stable renal, cardiac, and hepatic function. Furthermore, we highlight the diagnostic challenge of portal hypertension, which was characterized by discrepancies between HVPG and SAAG measurements. In systemic amyloidosis, where peritoneal involvement with ascites is uncommon, the primary therapeutic focus shifts to achieving a hematologic response and improving organ function, as demonstrated by our patient's clinical progression.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Zehra Naseem, MD1, Arjun Chatterjee, MD1, Muyiwa Awoniyi, MD2, Sandra Mazzoni, MD1, Sobia Laique, MD1. P4766 - Ascites as a Harbinger of Peritoneal and Hepatic Amyloidosis in AL Amyloidosis and Multiple Myeloma Intersection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2Digestive Disease Institute, Cleveland Clinic, Cleveland, OH
Introduction: Amyloidosis disrupts organ function by depositing amyloid fibrils. The clinical presentation varies depending on the type of amyloid and its accumulation site. While gastrointestinal symptoms are frequently observed, hepatic and peritoneal amyloidosis accompanied by ascites is uncommon. Here, we report a rare case of worsening ascites due to co-existing hepatic and peritoneal amyloidosis in a patient with multisystemic AL amyloidosis and multiple myeloma, detailing our management approach.
Case Description/Methods: A 53-year-old woman with multiple myeloma and biopsy-proven AL amyloidosis involving her liver (Figure 1A and 1B), heart, and bone marrow was hospitalized due to rapidly worsening ascites and shortness of breath. Despite six months of treatment with Daratumumab and CyBorD (as per the ANDROMEDA trial), supplemented by diuretics, her symptoms progressed, necessitating frequent paracentesis.
Chest X-rays ruled out pleural effusion, and no deterioration was observed in her cardiac, renal, or hepatic functions. Alkaline phosphatase levels remained chronically elevated at 900-1000 U/L, and the serum-ascites albumin gradient (SAAG) consistently exceeded 1.1 (Table 1), indicating portal hypertension. However, the hepatic venous pressure gradient (HVPG) was normal at 4, suggesting pre-sinusoidal congestion. An abdominal CT scan (Figure 1C) revealed omental and peritoneal fat stranding, consistent with amyloid infiltration.
The patient was discharged in stable condition with a treatment plan that included ongoing diuretics and scheduled paracentesis. She transitioned to a regimen of bortezomib, venetoclax, and daratumumab, which suppressed her light chain production, leading to improved ascites.
Discussion: Ascites in peritoneal amyloidosis is extremely rare, with only one reported case involving concurrent hepatic amyloidosis. Therefore, peritoneal involvement by amyloidosis should be considered in an ascitic patient with relatively stable renal, cardiac, and hepatic function. Furthermore, we highlight the diagnostic challenge of portal hypertension, which was characterized by discrepancies between HVPG and SAAG measurements. In systemic amyloidosis, where peritoneal involvement with ascites is uncommon, the primary therapeutic focus shifts to achieving a hematologic response and improving organ function, as demonstrated by our patient's clinical progression.
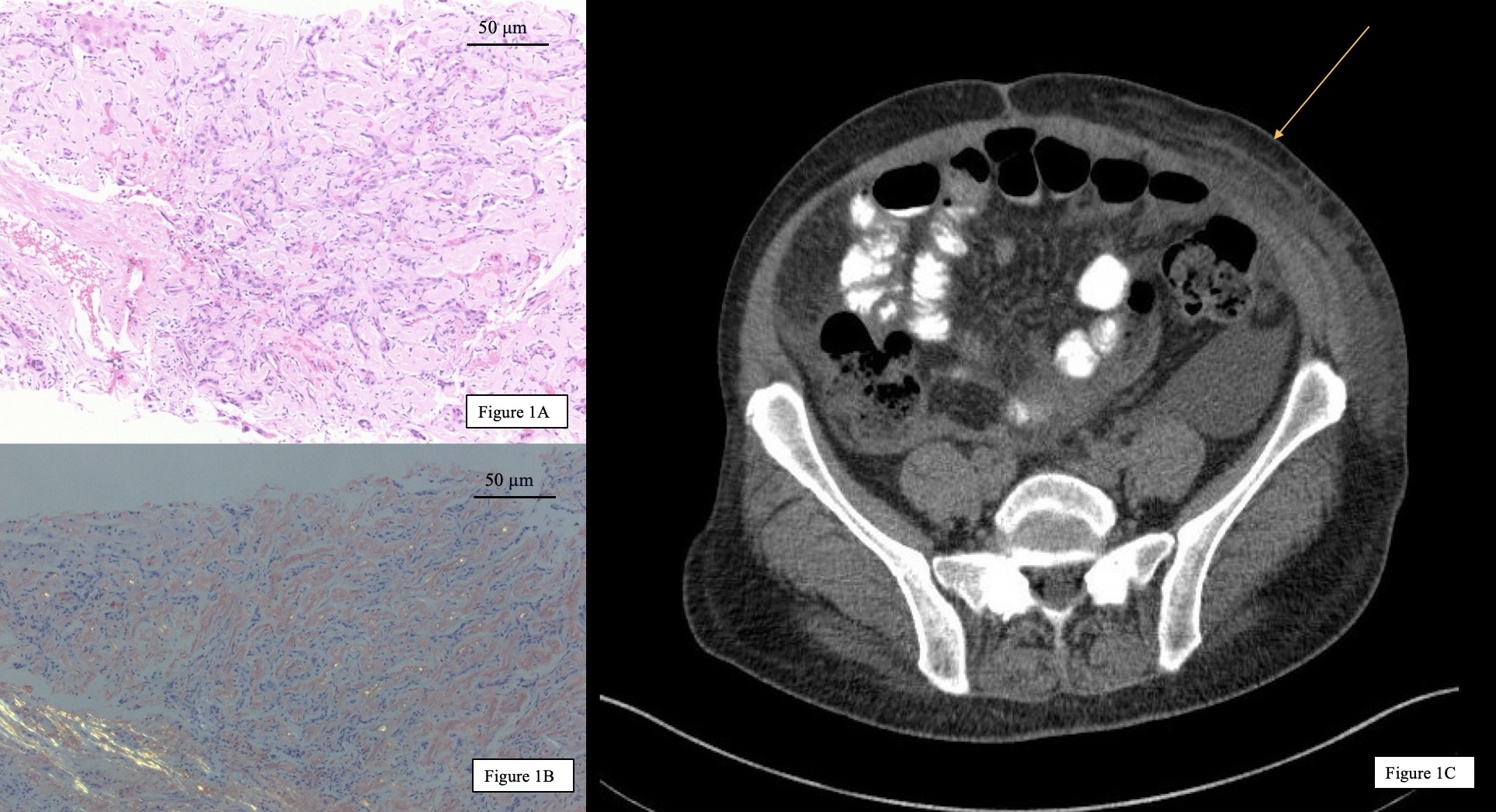
Figure: Figure 1A: Liver parenchyma with marked amyloid deposition, associated with areas of fibrous scar and ductular proliferation (hematoxylin and eosin, original magnification x 20)
Figure 1B: Apple-green birefringence under polarized light within sinusoids and portal tracts (Congo red staining original magnification x 20)
Figure 1C: Abdominal and pelvic CT scan without IV contrast showing omental and peritoneal fat stranding (yellow arrow)
Figure 1B: Apple-green birefringence under polarized light within sinusoids and portal tracts (Congo red staining original magnification x 20)
Figure 1C: Abdominal and pelvic CT scan without IV contrast showing omental and peritoneal fat stranding (yellow arrow)
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Zehra Naseem indicated no relevant financial relationships.
Arjun Chatterjee indicated no relevant financial relationships.
Muyiwa Awoniyi indicated no relevant financial relationships.
Sandra Mazzoni indicated no relevant financial relationships.
Sobia Laique indicated no relevant financial relationships.
Zehra Naseem, MD1, Arjun Chatterjee, MD1, Muyiwa Awoniyi, MD2, Sandra Mazzoni, MD1, Sobia Laique, MD1. P4766 - Ascites as a Harbinger of Peritoneal and Hepatic Amyloidosis in AL Amyloidosis and Multiple Myeloma Intersection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
