Tuesday Poster Session
Category: Liver
P4674 - Risk Factors for Hospital and ICU Admission in Patients Delisted for Liver Transplant
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Kai-Lou Yue, BS
University of Massachusetts Chan Medical School
Worcester, MA
Presenting Author(s)
Kai-Lou Yue, BS1, Katherine Cooper, MD1, Dhruval Amin, MD1, Daniel Belza, MD1, Neil Marya, MD2, Navine Nasser-Ghodsi, MD3
1University of Massachusetts Chan Medical School, Worcester, MA; 2University of Massachusetts Memorial Medical Center, Worcester, MA; 3UMass Chan Medical School & UMass Memorial Health Care, Worcester, MA
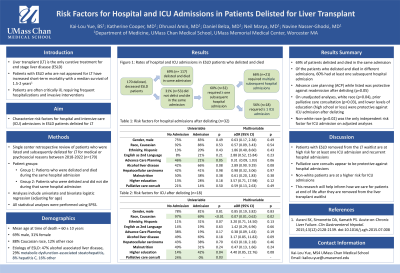
Introduction: Liver transplant (LT) is the only curative treatment for end stage liver disease (ESLD). Patients awaiting LT are often critically ill requiring frequent hospitalizations and invasive interventions. Patients with ESLD who are not approved for LT have a high rate of short-term mortality with a median survival of 1.5-2 years. We aimed to characterize risk factors for hospital and intensive care (ICU) admissions in ESLD patients delisted for LT.
Methods: We performed a single center retrospective review of consecutive patients who were listed and subsequently delisted for LT for medical or psychosocial reasons between 2018-2022. Two groups of patients were identified: patients who were delisted and 1) died during the same hospital admission and 2) did not die during the same admission. Factors associated with hospital and ICU admission after delisting were identified using Chi squared tests. Multivariable logistic regression was used to assess associations when controlling for age at delisting.
Results: A total of 170 patients with a mean age of 60 ± 10 years were included. Most patients (69%) delisted and died during the same admission. Of those who did not (n=53, 31%), 60% required at least one subsequent hospital admission. Multiple admissions were required in 21 (66%) patients, and 18 (56%) patients required ≥ 1 ICU admission. The following variables were associated with decreased odds of ICU admission after delisting: white race (p=0.04), more than high school education (p=0.04), prior advance care planning (ACP) (p=0.05), and prior palliative care (PC) consultation (p=0.03). On multivariable analysis, non-white race (p=0.02) was the only independent risk factor for ICU admission after delisting. The association of PC consult was unable to be assessed with multivariable regression, as none of the patients with a PC consult were admitted to the ICU after delisting compared to 36% of those without a PC consult.
Discussion: Patients with ESLD who are removed from the LT waitlist are at high risk for hospital admission, but PC consult appears protective against hospital admission. Conversely, non-white patients are at a higher risk for ICU admission. This research will help to inform how we care for patients at end of life after they are removed from the LT waitlist.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kai-Lou Yue, BS1, Katherine Cooper, MD1, Dhruval Amin, MD1, Daniel Belza, MD1, Neil Marya, MD2, Navine Nasser-Ghodsi, MD3. P4674 - Risk Factors for Hospital and ICU Admission in Patients Delisted for Liver Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Massachusetts Chan Medical School, Worcester, MA; 2University of Massachusetts Memorial Medical Center, Worcester, MA; 3UMass Chan Medical School & UMass Memorial Health Care, Worcester, MA
Introduction: Liver transplant (LT) is the only curative treatment for end stage liver disease (ESLD). Patients awaiting LT are often critically ill requiring frequent hospitalizations and invasive interventions. Patients with ESLD who are not approved for LT have a high rate of short-term mortality with a median survival of 1.5-2 years. We aimed to characterize risk factors for hospital and intensive care (ICU) admissions in ESLD patients delisted for LT.
Methods: We performed a single center retrospective review of consecutive patients who were listed and subsequently delisted for LT for medical or psychosocial reasons between 2018-2022. Two groups of patients were identified: patients who were delisted and 1) died during the same hospital admission and 2) did not die during the same admission. Factors associated with hospital and ICU admission after delisting were identified using Chi squared tests. Multivariable logistic regression was used to assess associations when controlling for age at delisting.
Results: A total of 170 patients with a mean age of 60 ± 10 years were included. Most patients (69%) delisted and died during the same admission. Of those who did not (n=53, 31%), 60% required at least one subsequent hospital admission. Multiple admissions were required in 21 (66%) patients, and 18 (56%) patients required ≥ 1 ICU admission. The following variables were associated with decreased odds of ICU admission after delisting: white race (p=0.04), more than high school education (p=0.04), prior advance care planning (ACP) (p=0.05), and prior palliative care (PC) consultation (p=0.03). On multivariable analysis, non-white race (p=0.02) was the only independent risk factor for ICU admission after delisting. The association of PC consult was unable to be assessed with multivariable regression, as none of the patients with a PC consult were admitted to the ICU after delisting compared to 36% of those without a PC consult.
Discussion: Patients with ESLD who are removed from the LT waitlist are at high risk for hospital admission, but PC consult appears protective against hospital admission. Conversely, non-white patients are at a higher risk for ICU admission. This research will help to inform how we care for patients at end of life after they are removed from the LT waitlist.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kai-Lou Yue indicated no relevant financial relationships.
Katherine Cooper indicated no relevant financial relationships.
Dhruval Amin indicated no relevant financial relationships.
Daniel Belza indicated no relevant financial relationships.
Neil Marya: Boston Scientific – Consultant.
Navine Nasser-Ghodsi: Boston Scientific – Consultant.
Kai-Lou Yue, BS1, Katherine Cooper, MD1, Dhruval Amin, MD1, Daniel Belza, MD1, Neil Marya, MD2, Navine Nasser-Ghodsi, MD3. P4674 - Risk Factors for Hospital and ICU Admission in Patients Delisted for Liver Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
