Tuesday Poster Session
Category: Liver
P4675 - Retreatment Following Initial Treatment With Terlipressin Improved Clinical Outcomes Among Patients With Hepatorenal Syndrome-Acute Kidney Injury: A Pooled Post Hoc Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Kimberly Brown, MD
Henry Ford Health
Detroit, MI
Presenting Author(s)
Kimberly Brown, MD1, Zachary P.. Fricker, MD2, Shehzad N.. Merwat, MD3, Manhal J.. Izzy, MD4, Sanaz Cardoza, PharmD5
1Henry Ford Health, Detroit, MI; 2Beth Israel Deaconess Medical Center, Boston, MA; 3The University of Texas Health Science Center at Houston, Houston, TX; 4Vanderbilt University, Nashville, TN; 5Mallinckrodt Pharmaceuticals, Bridgewater, NJ
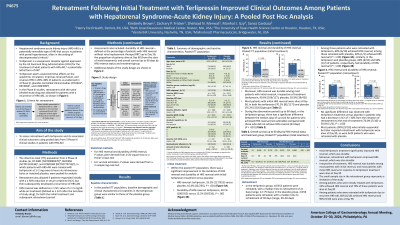
Introduction: Terlipressin is used to treat hepatorenal syndrome-acute kidney injury (HRS-AKI), a potentially lethal form of AKI. In 3 Phase III clinical studies of terlipressin treatment of patients with HRS-AKI, retreatment with the same blinded study drug was allowed for patients who initially responded to treatment with a ≥30% reduction in serum creatinine (SCr), but then met the HRS diagnosis criteria again (≤90 days from the first dose of study drug). This study assessed retreatment with terlipressin and its associated clinical outcomes using pooled data from the 3 Phase III clinical studies.
Methods: The intent-to-treat (ITT) population of 3 Phase III studies (ie, OT-0401, REVERSE, and CONFIRM), in which patients with HRS-AKI were treated with terlipressin at 1–2 mg every 6 hours via intravenous bolus or matched placebo, were pooled for the analysis. Retreatment was allowed if patients responded initially with a ≥30% reduction in SCr but then subsequently developed a recurrence of HRS-AKI. HRS reversal was defined as ≥1 SCr value of ≤1.5 mg/dL on treatment (≤24 h after the last dose of study drug), for both the initial treatment and subsequent retreatment period. Assessments also included: durable HRS reversal, defined as HRS reversal without renal replacement therapy up to Day 30; and the proportion of patients alive at Day 90 (from start of initial treatment).
Results: There was a significant improvement in HRS reversal and durable HRS reversal with initial terlipressin treatment versus placebo (HRS reversal: 33.2% [117/352] vs 16.4% [42/256], P< .001; durable HRS reversal, 30.1% [106/352] vs 15.2% [39/256], P< .001). Moreover, HRS reversal was durable among most patients with initial reversal (terlipressin, 90.6% [106/117]; placebo, 92.9% [39/42]). Ten patients eligible for retreatment with terlipressin were retreated, with a median time to retreatment of 21 days (range: 12–75 days). Among those retreated with terlipressin, 60% (6/10) achieved HRS reversal. Most patients (70.1% [82/117]) with initial HRS reversal in response to terlipressin treatment were alive at Day 90. Similarly, most patients (90% [9/10]) who initially responded but later required retreatment with terlipressin were also alive at Day 90.
Discussion: Terlipressin retreatment significantly improved HRS reversal, which was durable. Among patients eligible for retreatment with terlipressin due to recurrent HRS-AKI, 6/10 achieved HRS reversal and 9/10 were alive at Day 90.
Disclosures:
Kimberly Brown, MD1, Zachary P.. Fricker, MD2, Shehzad N.. Merwat, MD3, Manhal J.. Izzy, MD4, Sanaz Cardoza, PharmD5. P4675 - Retreatment Following Initial Treatment With Terlipressin Improved Clinical Outcomes Among Patients With Hepatorenal Syndrome-Acute Kidney Injury: A Pooled Post Hoc Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Health, Detroit, MI; 2Beth Israel Deaconess Medical Center, Boston, MA; 3The University of Texas Health Science Center at Houston, Houston, TX; 4Vanderbilt University, Nashville, TN; 5Mallinckrodt Pharmaceuticals, Bridgewater, NJ
Introduction: Terlipressin is used to treat hepatorenal syndrome-acute kidney injury (HRS-AKI), a potentially lethal form of AKI. In 3 Phase III clinical studies of terlipressin treatment of patients with HRS-AKI, retreatment with the same blinded study drug was allowed for patients who initially responded to treatment with a ≥30% reduction in serum creatinine (SCr), but then met the HRS diagnosis criteria again (≤90 days from the first dose of study drug). This study assessed retreatment with terlipressin and its associated clinical outcomes using pooled data from the 3 Phase III clinical studies.
Methods: The intent-to-treat (ITT) population of 3 Phase III studies (ie, OT-0401, REVERSE, and CONFIRM), in which patients with HRS-AKI were treated with terlipressin at 1–2 mg every 6 hours via intravenous bolus or matched placebo, were pooled for the analysis. Retreatment was allowed if patients responded initially with a ≥30% reduction in SCr but then subsequently developed a recurrence of HRS-AKI. HRS reversal was defined as ≥1 SCr value of ≤1.5 mg/dL on treatment (≤24 h after the last dose of study drug), for both the initial treatment and subsequent retreatment period. Assessments also included: durable HRS reversal, defined as HRS reversal without renal replacement therapy up to Day 30; and the proportion of patients alive at Day 90 (from start of initial treatment).
Results: There was a significant improvement in HRS reversal and durable HRS reversal with initial terlipressin treatment versus placebo (HRS reversal: 33.2% [117/352] vs 16.4% [42/256], P< .001; durable HRS reversal, 30.1% [106/352] vs 15.2% [39/256], P< .001). Moreover, HRS reversal was durable among most patients with initial reversal (terlipressin, 90.6% [106/117]; placebo, 92.9% [39/42]). Ten patients eligible for retreatment with terlipressin were retreated, with a median time to retreatment of 21 days (range: 12–75 days). Among those retreated with terlipressin, 60% (6/10) achieved HRS reversal. Most patients (70.1% [82/117]) with initial HRS reversal in response to terlipressin treatment were alive at Day 90. Similarly, most patients (90% [9/10]) who initially responded but later required retreatment with terlipressin were also alive at Day 90.
Discussion: Terlipressin retreatment significantly improved HRS reversal, which was durable. Among patients eligible for retreatment with terlipressin due to recurrent HRS-AKI, 6/10 achieved HRS reversal and 9/10 were alive at Day 90.
Disclosures:
Kimberly Brown: Mallinckrodt, Gilead, salix, Ipsen, intercept, madrigal, alexion – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau.
Zachary Fricker: Bausch, Inc – Grant/Research Support. Lipocine, Inc – Grant/Research Support. River2Renal Corp – Grant/Research Support.
Shehzad Merwat: AbbVie – Speakers Bureau.
Manhal Izzy: Mallinckrodt – Speakers Bureau.
Sanaz Cardoza: Mallinckrodt Pharmaceuticals – Employee, Stock-publicly held company(excluding mutual/index funds).
Kimberly Brown, MD1, Zachary P.. Fricker, MD2, Shehzad N.. Merwat, MD3, Manhal J.. Izzy, MD4, Sanaz Cardoza, PharmD5. P4675 - Retreatment Following Initial Treatment With Terlipressin Improved Clinical Outcomes Among Patients With Hepatorenal Syndrome-Acute Kidney Injury: A Pooled Post Hoc Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
