Tuesday Poster Session
Category: Liver
P4677 - Clinical Outcomes in Metabolic Dysfunction-Associated Fatty Liver Disease Patients Admitted With Acute Respiratory Failure
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Fernando R. Mateo, MD
TriHealth Good Samaritan Hospital
Cincinnati, OH
Presenting Author(s)
Fernando R. Mateo, MD1, M Kenan Rahima, MD1, Mhd Kutaiba Albuni, MD2, Tochukwu Ikpeze, MD, MBA, MS3, Venkata Muddana, MD4
1TriHealth Good Samaritan Hospital, Cincinnati, OH; 2TriHealth, Doha, Ad Dawhah, Qatar; 3TriHealth, CIncinatti, OH; 4TriHealth, Cincinnati, OH
Introduction: Acute Respiratory Failure (ARF) and Metabolic Dysfunction Associated Fatty Liver Disease (MAFLD) are characterized by systemic inflammation. Acute respiratory distress syndrome (ARDS), initiates a systemic inflammatory response affecting multiple organs. MAFLD is associated with low-grade systemic inflammation. There's limited evidence examining the outcomes of patients presenting with both ARF and MAFLD. Our objective was to assess clinical outcomes in this population.
Methods: We accessed the National Inpatient Sample from 2017-2020 to identify adults with MAFLD hospitalized with ARF. The primary endpoint was inpatient mortality, with secondary endpoints of cardiogenic shock, cardiac arrest, gastrointestinal bleeding (GIB), length of stay (LOS), and hospital charges. We utilized multivariable logistic regression analysis to estimate clinical outcomes, considering a threshold of P < 0.05.
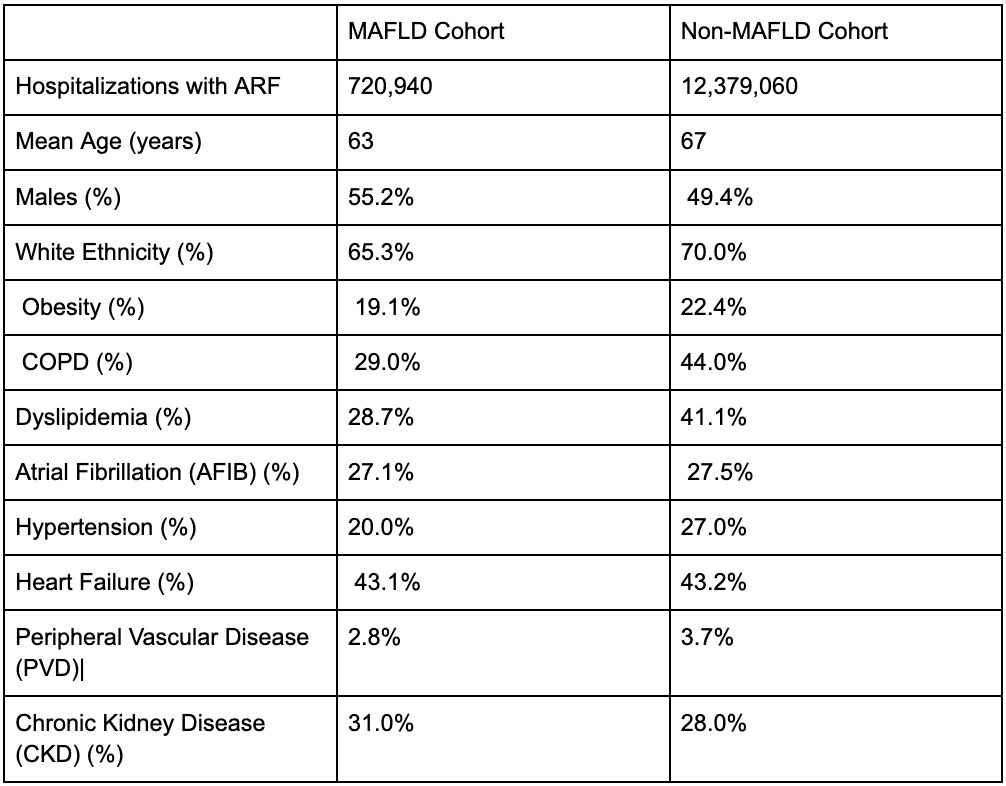
Results: We identified 13,100,000 hospitalizations with ARF, 720,940 (5.5%) presented MAFLD. Comparing MAFLD and Non-MAFLD cohorts, mean age was 63 vs 67 years, males 55.2% vs 49.4%, and White ethnicity 65.3% vs 70%. The prevalence of obesity was 19.1% vs 22.4%, chronic obstructive pulmonary disease (COPD) 29% vs 44%, dyslipidemia 28.7% vs 41.1%, atrial fibrillation (AFIB) 27.1% vs 27.5%, hypertension 20% vs 27%, heart failure 43.1% vs 43.2%, peripheral vascular disease (PVD) 2.8% vs 3.7%, and chronic kidney disease (CKD) 31% vs 28%. Clinical outcomes between cohorts: in-hospital mortality rates were 37.6% vs 12.1% with an odds ratio (OR) of 4.77 (CI 4.69-4.84); Cardiogenic shock rate 13.6% vs 2.6% (OR 4.55, CI 4.44-4.66); Cardiac arrest rates 14.3% vs 3.96% with OR 3.46 (CI 3.38–3.54); Intensive care need 43.1% vs 18.6% with an OR of 2.7 (CI 2.68-2.77); GI bleeding 12.3% vs 4% (OR 2.94, CI 2.89-3.0); LOS 11.3 days vs 8.2 days (IRR 1.2, CI 1.19-1.22); and hospital charges were 47,847 vs 25,377 (IRR 1.56, CI 1.54-1.58). All data with a p-value < 0.001 and adjusted for various factors including age, sex, race, comorbidity indices, ARF, and inflation during 2017-2020.
Discussion: Patients hospitalized for ARF and MAFLD were younger, with fewer females and Caucasians. They exhibited less obesity, AFIB, COPD, or PVD. Importantly, they showed worse clinical outcomes, including higher mortality rates, adverse events (GIB, cardiac arrest, cardiogenic shock), prolonged LOS, and increased resource utilization. Clinicians should consider MAFLD as a negative predictor when managing patients with ARF.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Fernando R. Mateo, MD1, M Kenan Rahima, MD1, Mhd Kutaiba Albuni, MD2, Tochukwu Ikpeze, MD, MBA, MS3, Venkata Muddana, MD4. P4677 - Clinical Outcomes in Metabolic Dysfunction-Associated Fatty Liver Disease Patients Admitted With Acute Respiratory Failure, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1TriHealth Good Samaritan Hospital, Cincinnati, OH; 2TriHealth, Doha, Ad Dawhah, Qatar; 3TriHealth, CIncinatti, OH; 4TriHealth, Cincinnati, OH
Introduction: Acute Respiratory Failure (ARF) and Metabolic Dysfunction Associated Fatty Liver Disease (MAFLD) are characterized by systemic inflammation. Acute respiratory distress syndrome (ARDS), initiates a systemic inflammatory response affecting multiple organs. MAFLD is associated with low-grade systemic inflammation. There's limited evidence examining the outcomes of patients presenting with both ARF and MAFLD. Our objective was to assess clinical outcomes in this population.
Methods: We accessed the National Inpatient Sample from 2017-2020 to identify adults with MAFLD hospitalized with ARF. The primary endpoint was inpatient mortality, with secondary endpoints of cardiogenic shock, cardiac arrest, gastrointestinal bleeding (GIB), length of stay (LOS), and hospital charges. We utilized multivariable logistic regression analysis to estimate clinical outcomes, considering a threshold of P < 0.05.
Results: We identified 13,100,000 hospitalizations with ARF, 720,940 (5.5%) presented MAFLD. Comparing MAFLD and Non-MAFLD cohorts, mean age was 63 vs 67 years, males 55.2% vs 49.4%, and White ethnicity 65.3% vs 70%. The prevalence of obesity was 19.1% vs 22.4%, chronic obstructive pulmonary disease (COPD) 29% vs 44%, dyslipidemia 28.7% vs 41.1%, atrial fibrillation (AFIB) 27.1% vs 27.5%, hypertension 20% vs 27%, heart failure 43.1% vs 43.2%, peripheral vascular disease (PVD) 2.8% vs 3.7%, and chronic kidney disease (CKD) 31% vs 28%. Clinical outcomes between cohorts: in-hospital mortality rates were 37.6% vs 12.1% with an odds ratio (OR) of 4.77 (CI 4.69-4.84); Cardiogenic shock rate 13.6% vs 2.6% (OR 4.55, CI 4.44-4.66); Cardiac arrest rates 14.3% vs 3.96% with OR 3.46 (CI 3.38–3.54); Intensive care need 43.1% vs 18.6% with an OR of 2.7 (CI 2.68-2.77); GI bleeding 12.3% vs 4% (OR 2.94, CI 2.89-3.0); LOS 11.3 days vs 8.2 days (IRR 1.2, CI 1.19-1.22); and hospital charges were 47,847 vs 25,377 (IRR 1.56, CI 1.54-1.58). All data with a p-value < 0.001 and adjusted for various factors including age, sex, race, comorbidity indices, ARF, and inflation during 2017-2020.
Discussion: Patients hospitalized for ARF and MAFLD were younger, with fewer females and Caucasians. They exhibited less obesity, AFIB, COPD, or PVD. Importantly, they showed worse clinical outcomes, including higher mortality rates, adverse events (GIB, cardiac arrest, cardiogenic shock), prolonged LOS, and increased resource utilization. Clinicians should consider MAFLD as a negative predictor when managing patients with ARF.
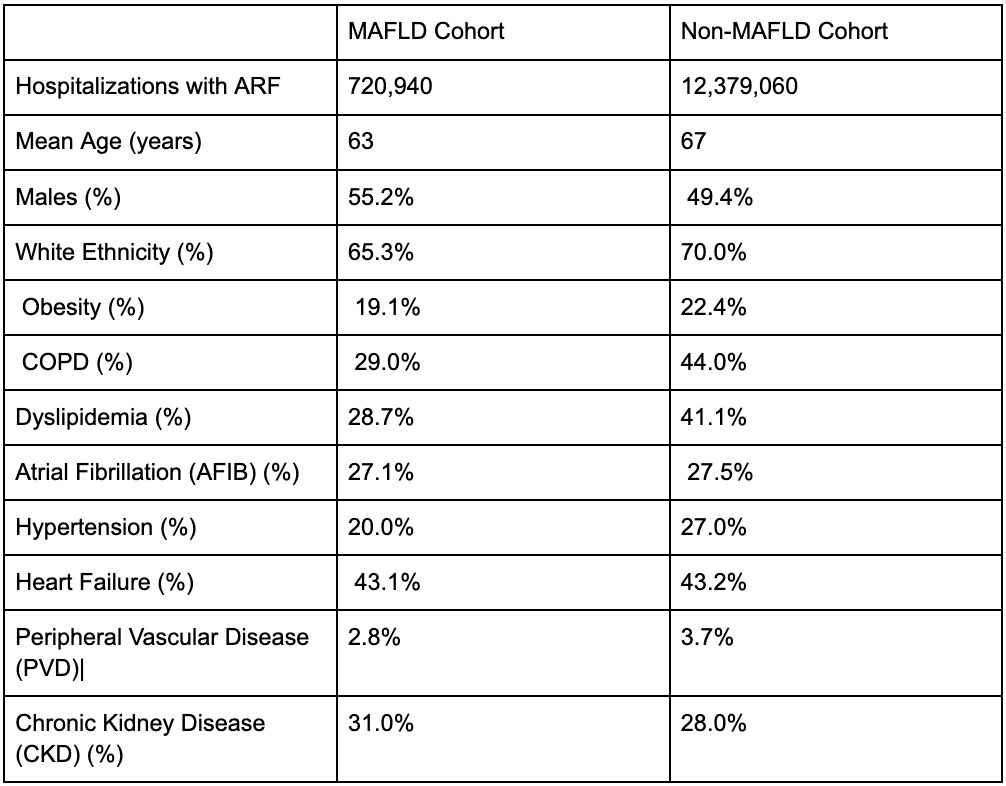
Figure: Patients baseline characteristics
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Fernando Mateo indicated no relevant financial relationships.
M Kenan Rahima indicated no relevant financial relationships.
Mhd Kutaiba Albuni indicated no relevant financial relationships.
Tochukwu Ikpeze indicated no relevant financial relationships.
Venkata Muddana indicated no relevant financial relationships.
Fernando R. Mateo, MD1, M Kenan Rahima, MD1, Mhd Kutaiba Albuni, MD2, Tochukwu Ikpeze, MD, MBA, MS3, Venkata Muddana, MD4. P4677 - Clinical Outcomes in Metabolic Dysfunction-Associated Fatty Liver Disease Patients Admitted With Acute Respiratory Failure, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
