Tuesday Poster Session
Category: Liver
P4681 - Risk of Portal Vein Thrombosis After Bariatric Surgery: Insights From a Propensity-Matched Study in the United States
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- OH
Osama Hamid, MD
University of Texas Southwestern Medical Center
Dallas, TX
Presenting Author(s)
Osama Hamid, MD1, Azizullah Beran, MD2, Mouhand F.H. Mohamed, MD, MSc3, Mohanad Awadalla, MD4, John Guardiola, MD2, Indira Bhavsar-Burke, MD, MHPE1
1University of Texas Southwestern Medical Center, Dallas, TX; 2Indiana University School of Medicine, Indianapolis, IN; 3Mayo Clinic, Rochester, MN; 4Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Bariatric surgery is an effective way to treat obesity and its related conditions. Portal vein thrombosis (PVT) has been observed following laparoscopic surgeries, with increasing reports of PVT after bariatric procedures. Our aim is to evaluate the risk of PVT following bariatric surgery compared to obese patients undergoing laparoscopic cholecystectomy (LC).
Methods: We conducted a retrospective cohort study utilizing a large dataset (TriNetX). We identified adults and selected 2 groups: patients who had bariatric surgery with no history of cirrhosis (study), and obese patients (BMI >30) who had LC with no cirrhosis or bariatric surgery (control). We performed 1:1 propensity-score matching (PSM) for demographics, comorbidities, thrombosis risk factors, post-operative complications (leak, obstruction, infection) and anticoagulation use. The primary outcome was the risk of PVT and venous thromboembolism (VTE), i.e deep vein thrombosis and pulmonary embolism, within 90 days of the procedure. Subgroup analysis was performed for the type of bariatric surgery. We evaluated the 8-year risk of portal hypertension (PHT) and esophageal varices (EV) in the bariatric group with PVT. Odds ratios (OR) with 95% confidence intervals (CI) were calculated to express the risk of each variable. A p-value of < 0.05 was considered statistically significant.
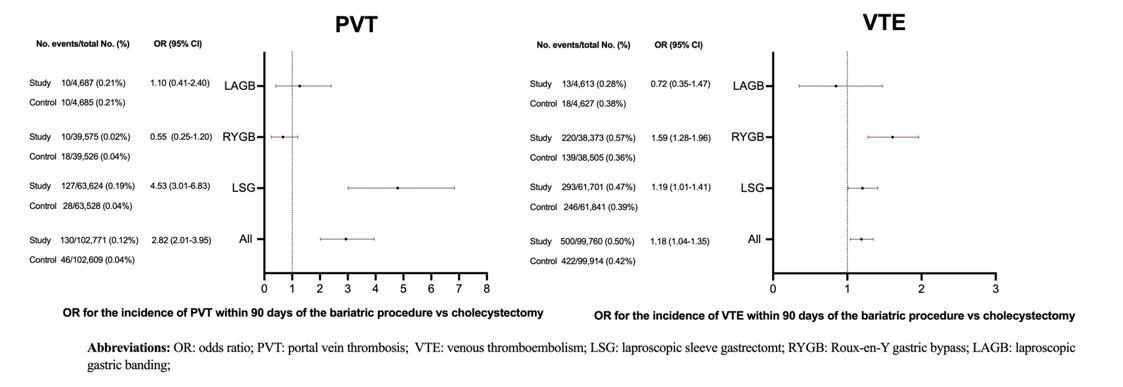
Results: A total of 112,040 patients were identified in the study group and 222,777 in control. The demographic profile and comorbidities are detailed in Table 1. After PSM, the bariatric surgery group had a higher risk of PVT (OR 2.82 [2.01-3.95]) and VTE (OR 1.18 [1.04-1.35]) compared to LC group. In subgroup analysis, sleeve gastrectomy (LSG) was associated with a significant risk of PVT (OR 4.53 [3.01-6.83]) and VTE (OR 1.19 [1.01-1.41]). Roux-en-Y gastric bypass (RYGB) showed no significant association with PVT (OR 0.55 [0.25-1.20]), but had a significant association with VTE (OR 1.59 [1.28-1.96]). Laparoscopic gastric banding (LAGB) showed no significant association with either PVT (OR 1.10 [0.41-2.40]) or VTE (OR 0.72 [0.35-1.47]), Fig 1. Among the bariatric group with PVT, the 8-year risk of PHT and EV was 6.57%.
Discussion: Bariatric surgery is associated with increased risk of PVT and VTE compared to a common laparoscopic surgery (LC). This risk was seen with LSG but not RYGB or LAGB, possibly attributed to vascular manipulation during LSG. Further studies are needed to assess the causality of the varying PVT risk among bariatric procedures.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Osama Hamid, MD1, Azizullah Beran, MD2, Mouhand F.H. Mohamed, MD, MSc3, Mohanad Awadalla, MD4, John Guardiola, MD2, Indira Bhavsar-Burke, MD, MHPE1. P4681 - Risk of Portal Vein Thrombosis After Bariatric Surgery: Insights From a Propensity-Matched Study in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Southwestern Medical Center, Dallas, TX; 2Indiana University School of Medicine, Indianapolis, IN; 3Mayo Clinic, Rochester, MN; 4Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Bariatric surgery is an effective way to treat obesity and its related conditions. Portal vein thrombosis (PVT) has been observed following laparoscopic surgeries, with increasing reports of PVT after bariatric procedures. Our aim is to evaluate the risk of PVT following bariatric surgery compared to obese patients undergoing laparoscopic cholecystectomy (LC).
Methods: We conducted a retrospective cohort study utilizing a large dataset (TriNetX). We identified adults and selected 2 groups: patients who had bariatric surgery with no history of cirrhosis (study), and obese patients (BMI >30) who had LC with no cirrhosis or bariatric surgery (control). We performed 1:1 propensity-score matching (PSM) for demographics, comorbidities, thrombosis risk factors, post-operative complications (leak, obstruction, infection) and anticoagulation use. The primary outcome was the risk of PVT and venous thromboembolism (VTE), i.e deep vein thrombosis and pulmonary embolism, within 90 days of the procedure. Subgroup analysis was performed for the type of bariatric surgery. We evaluated the 8-year risk of portal hypertension (PHT) and esophageal varices (EV) in the bariatric group with PVT. Odds ratios (OR) with 95% confidence intervals (CI) were calculated to express the risk of each variable. A p-value of < 0.05 was considered statistically significant.
Results: A total of 112,040 patients were identified in the study group and 222,777 in control. The demographic profile and comorbidities are detailed in Table 1. After PSM, the bariatric surgery group had a higher risk of PVT (OR 2.82 [2.01-3.95]) and VTE (OR 1.18 [1.04-1.35]) compared to LC group. In subgroup analysis, sleeve gastrectomy (LSG) was associated with a significant risk of PVT (OR 4.53 [3.01-6.83]) and VTE (OR 1.19 [1.01-1.41]). Roux-en-Y gastric bypass (RYGB) showed no significant association with PVT (OR 0.55 [0.25-1.20]), but had a significant association with VTE (OR 1.59 [1.28-1.96]). Laparoscopic gastric banding (LAGB) showed no significant association with either PVT (OR 1.10 [0.41-2.40]) or VTE (OR 0.72 [0.35-1.47]), Fig 1. Among the bariatric group with PVT, the 8-year risk of PHT and EV was 6.57%.
Discussion: Bariatric surgery is associated with increased risk of PVT and VTE compared to a common laparoscopic surgery (LC). This risk was seen with LSG but not RYGB or LAGB, possibly attributed to vascular manipulation during LSG. Further studies are needed to assess the causality of the varying PVT risk among bariatric procedures.
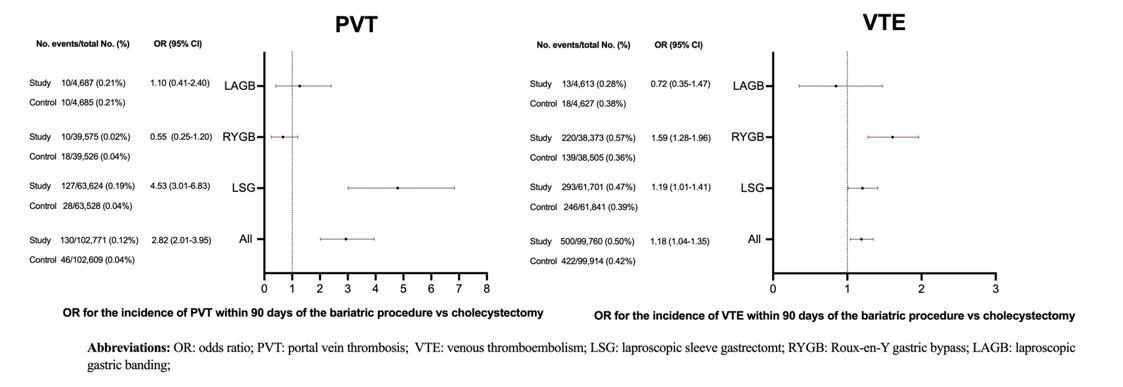
Figure: Figure 1: Risk of PVT and VTE after bariatric surgery procedures compared to laproscopic cholecystectomy in obese patients within 90 days of the procedure
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Osama Hamid indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Mouhand Mohamed indicated no relevant financial relationships.
Mohanad Awadalla indicated no relevant financial relationships.
John Guardiola: Boston Scientific Corporation – Travel Support. Olympus Corporation – Travel Support.
Indira Bhavsar-Burke indicated no relevant financial relationships.
Osama Hamid, MD1, Azizullah Beran, MD2, Mouhand F.H. Mohamed, MD, MSc3, Mohanad Awadalla, MD4, John Guardiola, MD2, Indira Bhavsar-Burke, MD, MHPE1. P4681 - Risk of Portal Vein Thrombosis After Bariatric Surgery: Insights From a Propensity-Matched Study in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
