Tuesday Poster Session
Category: Liver
P4682 - Maternal and Fetal Outcomes in Post-Transplant Pregnancies: Insights From a National Database
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Muhammad Ali Butt, MD
Allegheny General Hospital
Pittsburgh, PA
Presenting Author(s)
Muhammad Ali Butt, MD1, Himsikhar Khataniar, MD1, Sameen Aamer, MD1, Nabeeha Mohy-ud-din, MD2
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA
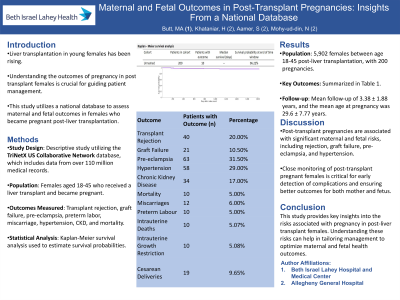
Introduction: There is an increasing incidence of liver transplants in younger females since the COVID pandemic. Pregnancy in females' post-transplantation presents unique challenges and risks. Understanding the outcomes associated with such pregnancies is crucial for optimizing patient care. This study aimed to comprehensively assess the various outcomes and risks in females who became pregnant post-liver transplantation using a multi-center national database.
Methods: A descriptive study was conducted utilizing data from Trinetx US Collaborative Network that contains de-identified data from 110 million medical records from 2006 onwards. The cohort comprised females who were liver transplant recipients and subsequently became pregnant. We assessed outcomes such as rejection, graft failure, pre-eclampsia, abortions, preterm labor, hypertension, chronic kidney disease (CKD), and mortality using ICD-10 codes. Kaplan-Meier survival analysis was employed to estimate survival probabilities.
Results: A total of 5,902 females aged 18-45 were identified post liver transplant, among which 200 pregnancies were recorded. The mean follow-up period was 3.38 ± 1.88 years, and the mean age at pregnancy was 29.6 ± 7.77 years. The rates of rejection and graft failure were 20% (n=40) and 10% (n=21), respectively. The rates of pre-eclampsia, pre-term labor, and miscarriages were 31% (n=63), 5% (n=10), and 6% (n=12), respectively. Additionally, 20% (n=58) were diagnosed with hypertension and 17% (n=34) with chronic kidney disease. The rates of intrauterine growth restriction, intrauterine deaths, and cesarean deliveries were 5% (n=10), 5% (n=10), and 9.7% (n=19), respectively. Mortality was observed in 5% (n=10).
Discussion: Pregnancy outcomes after liver transplant include risk of rejection and graft failure, along with a risk of preterm labor, preeclampsia, and miscarriages. These findings underscore the importance of close monitoring and tailored management strategies for pregnant females post liver transplantation to optimize maternal and fetal outcomes. Further research is warranted to elucidate underlying mechanisms and refine clinical management approaches.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Muhammad Ali Butt, MD1, Himsikhar Khataniar, MD1, Sameen Aamer, MD1, Nabeeha Mohy-ud-din, MD2. P4682 - Maternal and Fetal Outcomes in Post-Transplant Pregnancies: Insights From a National Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA
Introduction: There is an increasing incidence of liver transplants in younger females since the COVID pandemic. Pregnancy in females' post-transplantation presents unique challenges and risks. Understanding the outcomes associated with such pregnancies is crucial for optimizing patient care. This study aimed to comprehensively assess the various outcomes and risks in females who became pregnant post-liver transplantation using a multi-center national database.
Methods: A descriptive study was conducted utilizing data from Trinetx US Collaborative Network that contains de-identified data from 110 million medical records from 2006 onwards. The cohort comprised females who were liver transplant recipients and subsequently became pregnant. We assessed outcomes such as rejection, graft failure, pre-eclampsia, abortions, preterm labor, hypertension, chronic kidney disease (CKD), and mortality using ICD-10 codes. Kaplan-Meier survival analysis was employed to estimate survival probabilities.
Results: A total of 5,902 females aged 18-45 were identified post liver transplant, among which 200 pregnancies were recorded. The mean follow-up period was 3.38 ± 1.88 years, and the mean age at pregnancy was 29.6 ± 7.77 years. The rates of rejection and graft failure were 20% (n=40) and 10% (n=21), respectively. The rates of pre-eclampsia, pre-term labor, and miscarriages were 31% (n=63), 5% (n=10), and 6% (n=12), respectively. Additionally, 20% (n=58) were diagnosed with hypertension and 17% (n=34) with chronic kidney disease. The rates of intrauterine growth restriction, intrauterine deaths, and cesarean deliveries were 5% (n=10), 5% (n=10), and 9.7% (n=19), respectively. Mortality was observed in 5% (n=10).
Discussion: Pregnancy outcomes after liver transplant include risk of rejection and graft failure, along with a risk of preterm labor, preeclampsia, and miscarriages. These findings underscore the importance of close monitoring and tailored management strategies for pregnant females post liver transplantation to optimize maternal and fetal outcomes. Further research is warranted to elucidate underlying mechanisms and refine clinical management approaches.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Muhammad Ali Butt indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Sameen Aamer indicated no relevant financial relationships.
Nabeeha Mohy-ud-din indicated no relevant financial relationships.
Muhammad Ali Butt, MD1, Himsikhar Khataniar, MD1, Sameen Aamer, MD1, Nabeeha Mohy-ud-din, MD2. P4682 - Maternal and Fetal Outcomes in Post-Transplant Pregnancies: Insights From a National Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
