Tuesday Poster Session
Category: Liver
P4686 - Metabolic Syndrome Associated With Diastolic Dysfunction Predisposes to Transjugular Intrahepatic Portosystemic Shunt (TIPS) Failure in Cirrhosis With Refractory Ascites
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Yazan Abboud, MD
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Yazan Abboud, MD1, Jaspreet Suri, MD2, Ahmed Al-Khazraji, MD1, Kaveh Hajifathalian, MD1, Gordan Jiang, MD3, Raza Malik, MD4
1Rutgers New Jersey Medical School, Newark, NJ; 2Kaiser Permanente, Los Angeles, CA; 3Beth Israel Deaconess Medical Center, Boston, MA; 4Lahey Hospital and Medical Center, Burlington, MA
Introduction: Transjugular intrahepatic portosystemic shunt (TIPS) placement is used to manage refractory ascites in decompensated cirrhosis. Given that TIPS can increase cardiac output, evaluation of cardiac function is essential prior to TIPS. While prior literature showed that TIPS can pre-dispose to diastolic dysfunction (DD), there is limited data on the impact of DD on TIPS success. Therefore, we aimed to assess whether DD increases risk of TIPS failure.
Methods: This is a retrospective study at a tertiary medical center including all consecutive patients who underwent TIPS for refractory ascites between 2003-2015. Exclusion criteria included TIPS performed for an etiology besides refractory ascites, revised TIPS, and patients lost to follow-up 90 days post-TIPS. Data were collected at index admission for TIPS placement. Transthoracic echocardiogram was performed along with the ratio of peak early ventricular filling velocity (E) to late diastolic ventricular filling velocity (A) (E/A< 1). TIPS success was defined as a decrease in paracentesis frequency at 90-day follow-up post TIPS with resolution of any ascites or hepatic hydrothorax; TIPS failure was defined by the presence of ascites or hepatic hydrothorax at 90-day follow-up.
Results: 85 patients with cirrhosis met inclusion criteria (74% males, mean age 59 years) (Table). The most common cirrhosis etiology was alcoholic cirrhosis (35%) followed by Hepatitis C Virus (HCV) (24%) and Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) (13%). 53 patients had an E/A ratio > 1 (62%). 30 out of the 32 (95%) patients with a low E/A ratio (< 1) had alcohol and MASLD as cirrhosis etiology.
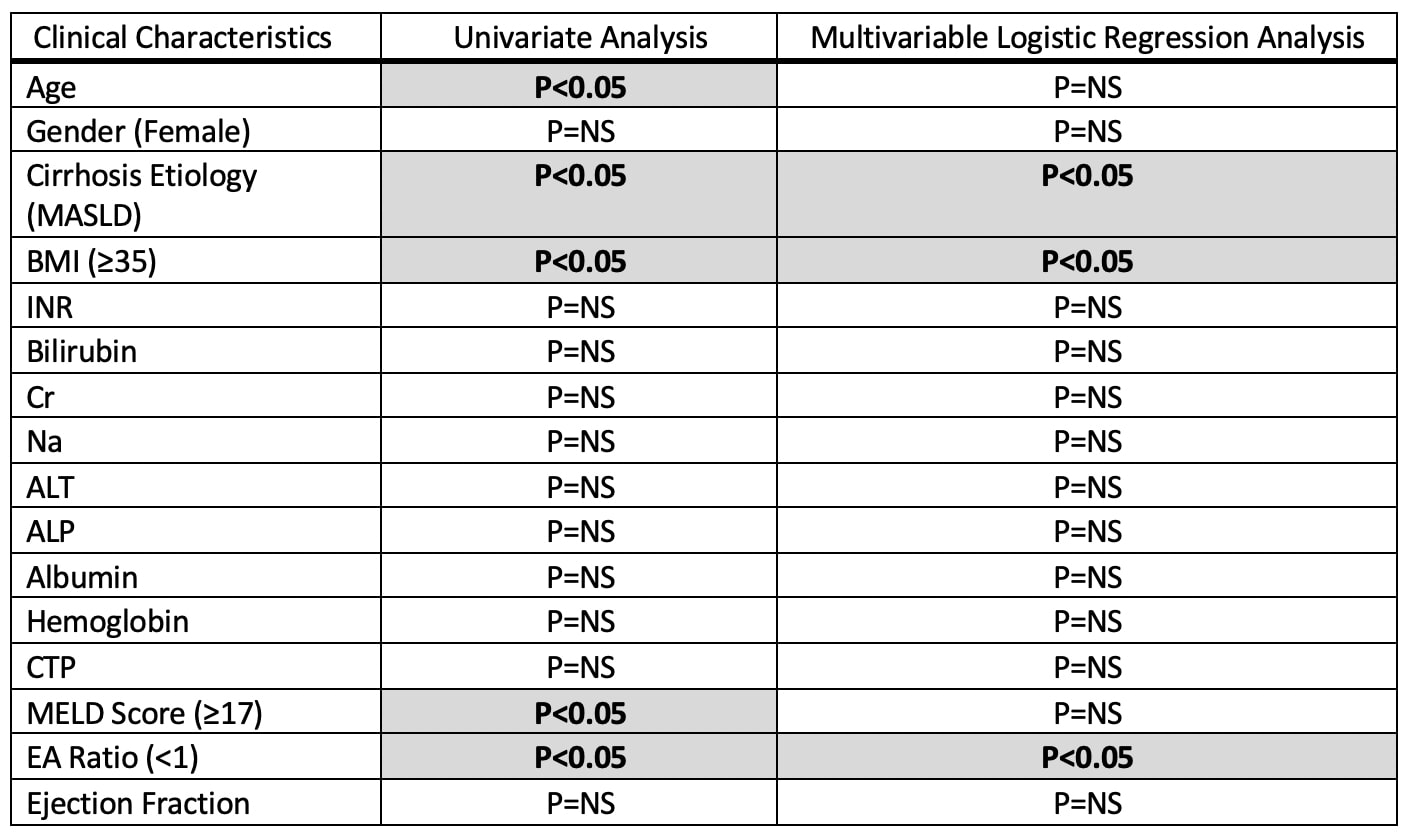
There were 17/85 (20%) patients who had TIPS failure. In univariate analysis: age >65 (P< 0.05), MASLD etiology (P< 0.05), BMI ≥35 (P< 0.05), E/A < 1 (P< 0.05), and MELD score ≥17 (P< 0.05) were predictive of TIPS failure (Figure). On multivariable analysis, after adjusting for the aforementioned significant variables, BMI ≥35 (odds ratio “OR” 2.2; P< 0.05), MASLD etiology (OR 2.56; P< 0.05), and E/A ratio < 1 (OR 3.0; P< 0.05) were associated with higher risk of TIPS failure (Figure).
Discussion: Diastolic cardiac dysfunction, obesity, and MASLD independently predict TIPS failure in patients with refractory ascites. Our results can aid clinicians in identifying patients at risk for TIPS failure to help in better addressing those comorbidities which can potentially improve TIPS outcomes. Future studies are warranted to externally validate our findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Yazan Abboud, MD1, Jaspreet Suri, MD2, Ahmed Al-Khazraji, MD1, Kaveh Hajifathalian, MD1, Gordan Jiang, MD3, Raza Malik, MD4. P4686 - Metabolic Syndrome Associated With Diastolic Dysfunction Predisposes to Transjugular Intrahepatic Portosystemic Shunt (TIPS) Failure in Cirrhosis With Refractory Ascites, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Newark, NJ; 2Kaiser Permanente, Los Angeles, CA; 3Beth Israel Deaconess Medical Center, Boston, MA; 4Lahey Hospital and Medical Center, Burlington, MA
Introduction: Transjugular intrahepatic portosystemic shunt (TIPS) placement is used to manage refractory ascites in decompensated cirrhosis. Given that TIPS can increase cardiac output, evaluation of cardiac function is essential prior to TIPS. While prior literature showed that TIPS can pre-dispose to diastolic dysfunction (DD), there is limited data on the impact of DD on TIPS success. Therefore, we aimed to assess whether DD increases risk of TIPS failure.
Methods: This is a retrospective study at a tertiary medical center including all consecutive patients who underwent TIPS for refractory ascites between 2003-2015. Exclusion criteria included TIPS performed for an etiology besides refractory ascites, revised TIPS, and patients lost to follow-up 90 days post-TIPS. Data were collected at index admission for TIPS placement. Transthoracic echocardiogram was performed along with the ratio of peak early ventricular filling velocity (E) to late diastolic ventricular filling velocity (A) (E/A< 1). TIPS success was defined as a decrease in paracentesis frequency at 90-day follow-up post TIPS with resolution of any ascites or hepatic hydrothorax; TIPS failure was defined by the presence of ascites or hepatic hydrothorax at 90-day follow-up.
Results: 85 patients with cirrhosis met inclusion criteria (74% males, mean age 59 years) (Table). The most common cirrhosis etiology was alcoholic cirrhosis (35%) followed by Hepatitis C Virus (HCV) (24%) and Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) (13%). 53 patients had an E/A ratio > 1 (62%). 30 out of the 32 (95%) patients with a low E/A ratio (< 1) had alcohol and MASLD as cirrhosis etiology.
There were 17/85 (20%) patients who had TIPS failure. In univariate analysis: age >65 (P< 0.05), MASLD etiology (P< 0.05), BMI ≥35 (P< 0.05), E/A < 1 (P< 0.05), and MELD score ≥17 (P< 0.05) were predictive of TIPS failure (Figure). On multivariable analysis, after adjusting for the aforementioned significant variables, BMI ≥35 (odds ratio “OR” 2.2; P< 0.05), MASLD etiology (OR 2.56; P< 0.05), and E/A ratio < 1 (OR 3.0; P< 0.05) were associated with higher risk of TIPS failure (Figure).
Discussion: Diastolic cardiac dysfunction, obesity, and MASLD independently predict TIPS failure in patients with refractory ascites. Our results can aid clinicians in identifying patients at risk for TIPS failure to help in better addressing those comorbidities which can potentially improve TIPS outcomes. Future studies are warranted to externally validate our findings.
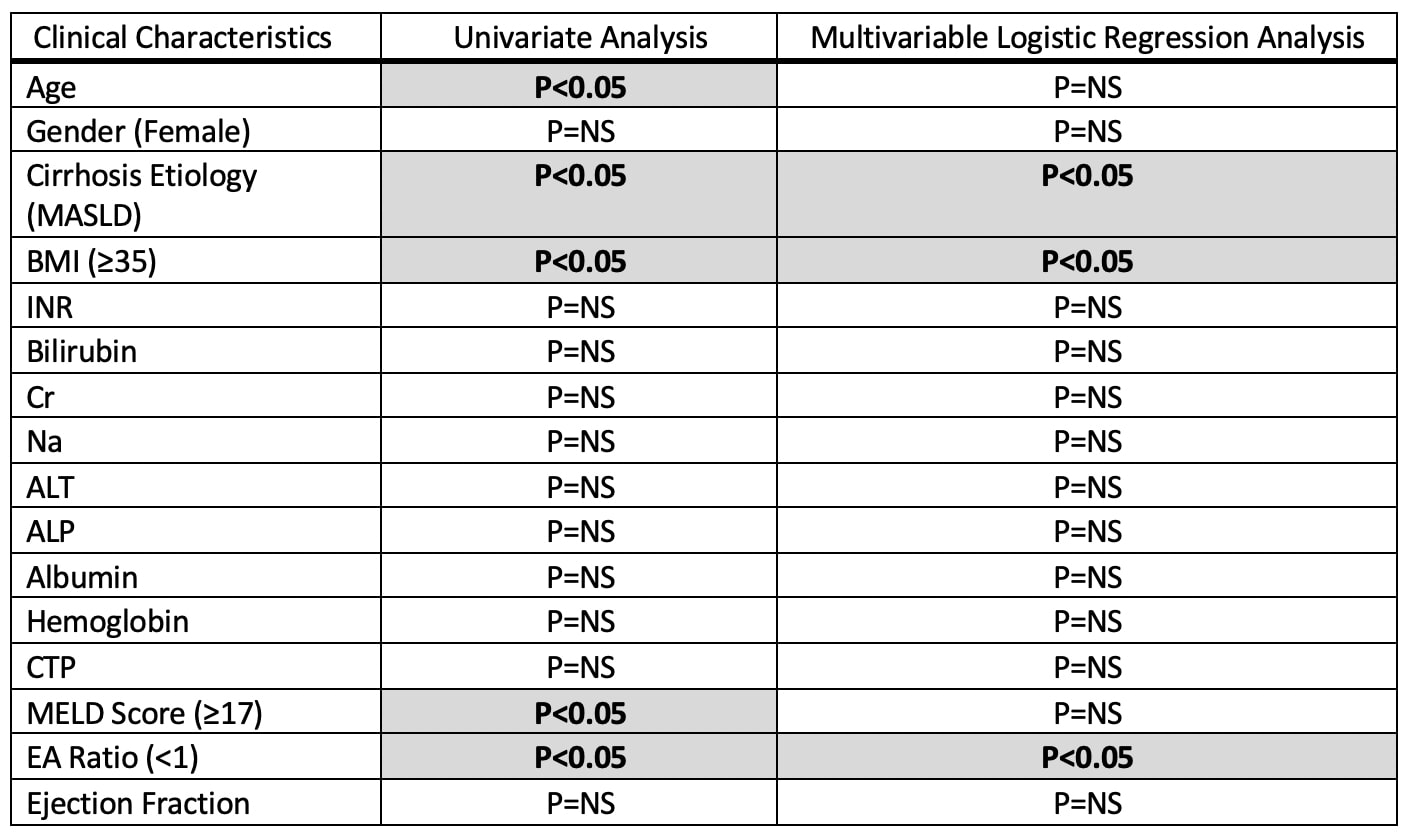
Figure: Figure: Clinical Predictors of Transjugular Intrahepatic Portosystemic Shunt (TIPS) Dysfunction Using Univariate and Multivariable Analysis.
MASLD: Metabolic Dysfunction-Associated Steatotic Liver Disease, CTP: Child Pugh Score, E/A: peak early ventricular filling velocity (E) to late diastolic ventricular filling velocity (A).
MASLD: Metabolic Dysfunction-Associated Steatotic Liver Disease, CTP: Child Pugh Score, E/A: peak early ventricular filling velocity (E) to late diastolic ventricular filling velocity (A).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Yazan Abboud indicated no relevant financial relationships.
Jaspreet Suri indicated no relevant financial relationships.
Ahmed Al-Khazraji indicated no relevant financial relationships.
Kaveh Hajifathalian indicated no relevant financial relationships.
Gordan Jiang indicated no relevant financial relationships.
Raza Malik indicated no relevant financial relationships.
Yazan Abboud, MD1, Jaspreet Suri, MD2, Ahmed Al-Khazraji, MD1, Kaveh Hajifathalian, MD1, Gordan Jiang, MD3, Raza Malik, MD4. P4686 - Metabolic Syndrome Associated With Diastolic Dysfunction Predisposes to Transjugular Intrahepatic Portosystemic Shunt (TIPS) Failure in Cirrhosis With Refractory Ascites, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
