Tuesday Poster Session
Category: Liver
P4581 - Don’t Get Confused – Prophylactic Lactulose Reduces Hepatic Encephalopathy and Hospital Admissions in Post-TIPS Patients
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- CE
Charles D. Evers, III, MD, MBA
University of Alabama at Birmingham Heersink School of Medicine
Homewood, AL
Presenting Author(s)
Charles D. Evers, MD, MBA1, Dalton A.. Norwood, MD2, Ethan D. Pollack, MS, MD3, John A. Cooper, MD3, Parth Patel, MD4, David Fettig, MD5
1University of Alabama at Birmingham Heersink School of Medicine, Homewood, AL; 2UAB Minority Health & Health Equity Research Center, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 3University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 4University of Alabama at Birmingham, Birmingham, AL; 5Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
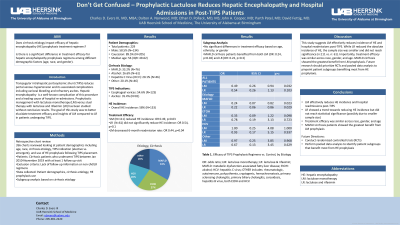
Introduction: Transjugular intrahepatic portosystemic shunt (TIPS) reduces portal venous hypertension and its associated complications including variceal bleeding and refractory ascites. Hepatic encephalopathy (HE) is a well-known complication of this procedure and a leading cause of hospital re-admissions. Prophylactic management with lactulose monotherapy (LM) versus dual therapy with lactulose and rifaximin (LR) has been studied without conclusive results. The goal of this study was to better elucidate treatment efficacy and insights of LM compared to LR in patients undergoing TIPS.
Methods: A single center, retrospective review identified all patients with cirrhosis who underwent TIPS between Jan 2010-November 2019. Patients without follow up information or on regimens other than LM or LR were excluded. Patient demographics, cirrhosis etiology, and use of HE prophylaxis following TIPS placement were identified. Subgroup analysis based on cirrhosis etiology was completed.
Results: Overall, the study included 229 patients. Males accounted for 58.5% (N=134) with a majority Caucasian cohort at 89.5% (N=205). The median age was 56 (IQR: 49-62). The most common cirrhosis etiology was MAFLD (N=76, 33.2%) followed by alcohol (N=61, 26.6%) and Hepatitis C Virus (HCV) (N=46, 20.1%). Esophageal varices (N=125, 54.6%) and ascites (N=81, 35.4%) were the most common indications for TIPS procedure. The incidence of HE was 58% (N=133) in the entire cohort. LM was more commonly administered (N=111) compared to LR (N=61). Overall, LM reduced incidence of HE (OR: 0.49, p=0.03), while LR did not (OR: 0.54, p=0.1). LM also decreased 6-month readmission rate following TIPS (OR:0.44, p=0.04). Subgroup analysis compared treatment arms LM and LR to age group, ethnicity, and gender and did not identify any significant differences between therapy groups. Interestingly, patients with MAFLD cirrhosis benefitted from both LM (OR: 0.24, p=0.02) and LR (OR: 0.22, p=0.3) while those with other etiologies did not within our cohort.
Discussion: This study suggests LM effectively reduces incidence of HE and hospital readmissions post-TIPS. While LR reduced the absolute incidence of HE, the sample size was smaller and did not reach significance (n:111 vs. n: 61). Importantly, treatment efficacy was similar across race, gender, and age. MAFLD cirrhosis showed the greatest benefit from LM prophylaxis. Future research should prioritize RCTs and pooled data analysis to pinpoint patient subgroups benefiting most from HE prophylaxis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Charles D. Evers, MD, MBA1, Dalton A.. Norwood, MD2, Ethan D. Pollack, MS, MD3, John A. Cooper, MD3, Parth Patel, MD4, David Fettig, MD5. P4581 - Don’t Get Confused – Prophylactic Lactulose Reduces Hepatic Encephalopathy and Hospital Admissions in Post-TIPS Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Alabama at Birmingham Heersink School of Medicine, Homewood, AL; 2UAB Minority Health & Health Equity Research Center, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 3University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 4University of Alabama at Birmingham, Birmingham, AL; 5Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Introduction: Transjugular intrahepatic portosystemic shunt (TIPS) reduces portal venous hypertension and its associated complications including variceal bleeding and refractory ascites. Hepatic encephalopathy (HE) is a well-known complication of this procedure and a leading cause of hospital re-admissions. Prophylactic management with lactulose monotherapy (LM) versus dual therapy with lactulose and rifaximin (LR) has been studied without conclusive results. The goal of this study was to better elucidate treatment efficacy and insights of LM compared to LR in patients undergoing TIPS.
Methods: A single center, retrospective review identified all patients with cirrhosis who underwent TIPS between Jan 2010-November 2019. Patients without follow up information or on regimens other than LM or LR were excluded. Patient demographics, cirrhosis etiology, and use of HE prophylaxis following TIPS placement were identified. Subgroup analysis based on cirrhosis etiology was completed.
Results: Overall, the study included 229 patients. Males accounted for 58.5% (N=134) with a majority Caucasian cohort at 89.5% (N=205). The median age was 56 (IQR: 49-62). The most common cirrhosis etiology was MAFLD (N=76, 33.2%) followed by alcohol (N=61, 26.6%) and Hepatitis C Virus (HCV) (N=46, 20.1%). Esophageal varices (N=125, 54.6%) and ascites (N=81, 35.4%) were the most common indications for TIPS procedure. The incidence of HE was 58% (N=133) in the entire cohort. LM was more commonly administered (N=111) compared to LR (N=61). Overall, LM reduced incidence of HE (OR: 0.49, p=0.03), while LR did not (OR: 0.54, p=0.1). LM also decreased 6-month readmission rate following TIPS (OR:0.44, p=0.04). Subgroup analysis compared treatment arms LM and LR to age group, ethnicity, and gender and did not identify any significant differences between therapy groups. Interestingly, patients with MAFLD cirrhosis benefitted from both LM (OR: 0.24, p=0.02) and LR (OR: 0.22, p=0.3) while those with other etiologies did not within our cohort.
Discussion: This study suggests LM effectively reduces incidence of HE and hospital readmissions post-TIPS. While LR reduced the absolute incidence of HE, the sample size was smaller and did not reach significance (n:111 vs. n: 61). Importantly, treatment efficacy was similar across race, gender, and age. MAFLD cirrhosis showed the greatest benefit from LM prophylaxis. Future research should prioritize RCTs and pooled data analysis to pinpoint patient subgroups benefiting most from HE prophylaxis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Charles Evers indicated no relevant financial relationships.
Dalton Norwood indicated no relevant financial relationships.
Ethan Pollack indicated no relevant financial relationships.
John Cooper indicated no relevant financial relationships.
Parth Patel indicated no relevant financial relationships.
David Fettig indicated no relevant financial relationships.
Charles D. Evers, MD, MBA1, Dalton A.. Norwood, MD2, Ethan D. Pollack, MS, MD3, John A. Cooper, MD3, Parth Patel, MD4, David Fettig, MD5. P4581 - Don’t Get Confused – Prophylactic Lactulose Reduces Hepatic Encephalopathy and Hospital Admissions in Post-TIPS Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
