Tuesday Poster Session
Category: Liver
P4586 - Are Asians and Pacific Islanders at Higher Risk? Insights From Hospitalized Patients With Cirrhosis Undergoing Paracentesis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Raj H. Patel, MD
St. Mary Medical Center
Bensalem, PA
Presenting Author(s)
Raj H. Patel, MD1, Charmy Parikh, MD2, Sneh Sonaiya, MD3, Umang Patel, MD4, Truptesh Kothari, MD5
1St. Mary Medical Center, Bensalem, PA; 2Mercy Catholic Medical Center, Darby, PA; 3University of Nevada, Las Vegas, NV; 4St. Mary Medical Center, Langhorne, PA; 5University of Rochester Medical Center, Rochester, NY
Introduction: Ascites, the most common complication of cirrhosis, develops in 5%-10% of patients each year and significantly impair quality of life. Paracentesis is minimally invasive with safe diagnostic and therapeutic benefits and is commonly utilized for the management of ascites in cirrhotic patients. However, it's important to note its potential for severe complications. Our study aims to examine the impact of racial disparities on outcomes among cirrhotic patients undergoing paracentesis.
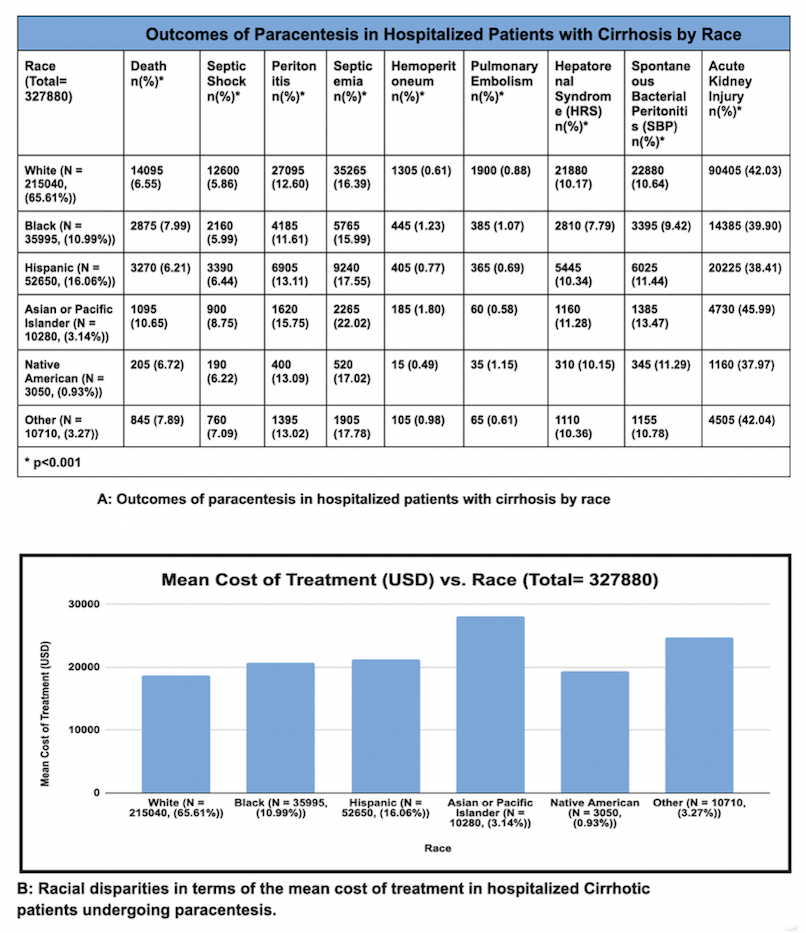
Methods: We conducted a retrospective analysis using the National Inpatient Sample (NIS) database from 2016 to 2020 to investigate how racial disparities impact outcomes in hospitalized liver cirrhosis patients undergoing paracentesis. Analysis was conducted using the SAS 9.4 software. Our study focused on mortality rates across different racial groups as the primary outcome. Secondary outcomes included assessing complications such as septic shock, peritonitis, septicemia, hemoperitoneum, pulmonary embolism, hepatorenal syndrome, spontaneous bacterial peritonitis (SBP), and acute kidney injury (AKI). Additionally, we analyzed the mean hospitalization costs and length of stay for these patients.
Results: 327,880 patients (46.34% female) with cirrhosis undergoing paracentesis across different racial groups were analyzed. Asian or Pacific Islander group (API) (3.14%) was associated with significantly high all-cause mortality compared to all other racial groups (OR: 1.658, 95% CI: 1.236 to 2.226, p< 0.001). For cirrhotic patients undergoing paracentesis, the API group was also associated with a higher incidence of complications such as septic shock (8.75%), peritonitis (15.75%), hemoperitoneum (1.80%), Hepatorenal syndrome (11.28%), Spontaneous Bacterial Peritonitis (13.47%), and acute kidney injury (45.99%) compared to other racial groups. There were significant differences in the mean cost of treatment and the length of hospital stay among different racial groups. The mean cost of treatment was $28,051 for API, $18,664 for White, and $20,782 for Black racial group. Additionally, the mean length of hospital stay for API, White, and Black patient groups was 8.05 days, 7.24 days, and 8.20 days respectively.
Discussion: The higher incidence of all-cause mortality and complications in the Asian or Pacific Islander group highlights the need for risk stratification and targeted intervention for patients with cirrhosis undergoing paracentesis.
Disclosures:
Raj H. Patel, MD1, Charmy Parikh, MD2, Sneh Sonaiya, MD3, Umang Patel, MD4, Truptesh Kothari, MD5. P4586 - Are Asians and Pacific Islanders at Higher Risk? Insights From Hospitalized Patients With Cirrhosis Undergoing Paracentesis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Mary Medical Center, Bensalem, PA; 2Mercy Catholic Medical Center, Darby, PA; 3University of Nevada, Las Vegas, NV; 4St. Mary Medical Center, Langhorne, PA; 5University of Rochester Medical Center, Rochester, NY
Introduction: Ascites, the most common complication of cirrhosis, develops in 5%-10% of patients each year and significantly impair quality of life. Paracentesis is minimally invasive with safe diagnostic and therapeutic benefits and is commonly utilized for the management of ascites in cirrhotic patients. However, it's important to note its potential for severe complications. Our study aims to examine the impact of racial disparities on outcomes among cirrhotic patients undergoing paracentesis.
Methods: We conducted a retrospective analysis using the National Inpatient Sample (NIS) database from 2016 to 2020 to investigate how racial disparities impact outcomes in hospitalized liver cirrhosis patients undergoing paracentesis. Analysis was conducted using the SAS 9.4 software. Our study focused on mortality rates across different racial groups as the primary outcome. Secondary outcomes included assessing complications such as septic shock, peritonitis, septicemia, hemoperitoneum, pulmonary embolism, hepatorenal syndrome, spontaneous bacterial peritonitis (SBP), and acute kidney injury (AKI). Additionally, we analyzed the mean hospitalization costs and length of stay for these patients.
Results: 327,880 patients (46.34% female) with cirrhosis undergoing paracentesis across different racial groups were analyzed. Asian or Pacific Islander group (API) (3.14%) was associated with significantly high all-cause mortality compared to all other racial groups (OR: 1.658, 95% CI: 1.236 to 2.226, p< 0.001). For cirrhotic patients undergoing paracentesis, the API group was also associated with a higher incidence of complications such as septic shock (8.75%), peritonitis (15.75%), hemoperitoneum (1.80%), Hepatorenal syndrome (11.28%), Spontaneous Bacterial Peritonitis (13.47%), and acute kidney injury (45.99%) compared to other racial groups. There were significant differences in the mean cost of treatment and the length of hospital stay among different racial groups. The mean cost of treatment was $28,051 for API, $18,664 for White, and $20,782 for Black racial group. Additionally, the mean length of hospital stay for API, White, and Black patient groups was 8.05 days, 7.24 days, and 8.20 days respectively.
Discussion: The higher incidence of all-cause mortality and complications in the Asian or Pacific Islander group highlights the need for risk stratification and targeted intervention for patients with cirrhosis undergoing paracentesis.
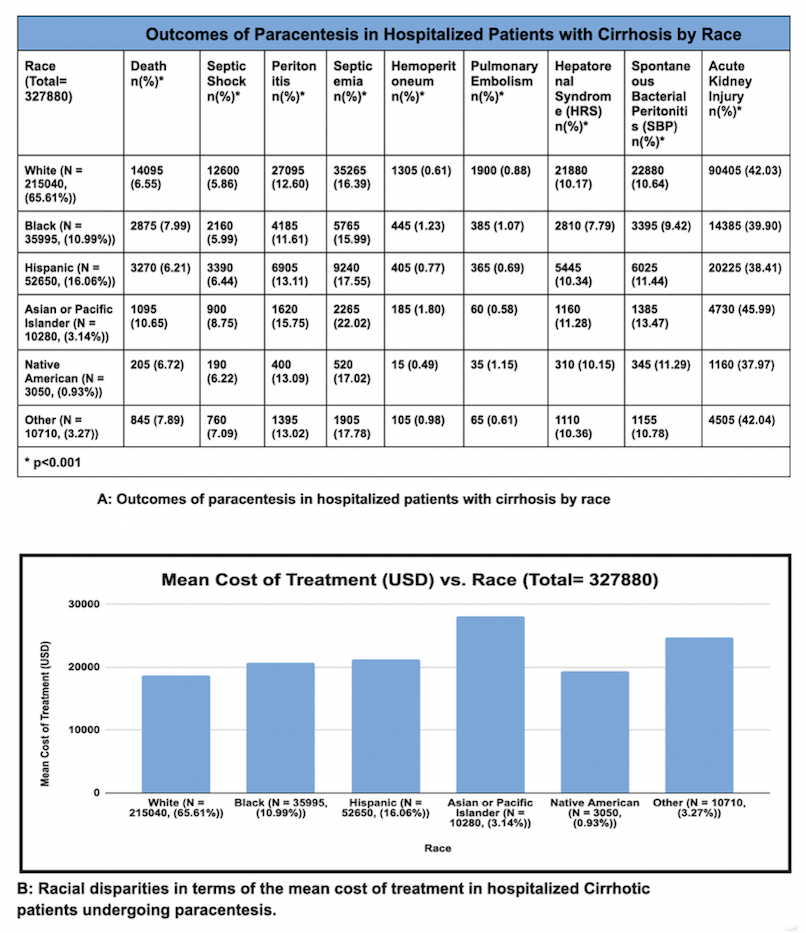
Figure: Ethnic Disparities in Cirrhotic Patient Outcomes: Mortality and Complications Following Paracentesis
Disclosures:
Raj Patel indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Umang Patel indicated no relevant financial relationships.
Truptesh Kothari indicated no relevant financial relationships.
Raj H. Patel, MD1, Charmy Parikh, MD2, Sneh Sonaiya, MD3, Umang Patel, MD4, Truptesh Kothari, MD5. P4586 - Are Asians and Pacific Islanders at Higher Risk? Insights From Hospitalized Patients With Cirrhosis Undergoing Paracentesis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
