Tuesday Poster Session
Category: Interventional Endoscopy
P4504 - Short Versus Standard Peroral Endoscopic Myotomy for Esophageal Achalasia: A Meta-Analysis of Randomized Controlled Trials
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- HA
Hashem Albunni, MD
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
Hashem Albunni, MD, Azizullah Beran, MD, Nwal Hadaki, MD, John M. DeWitt, MD, FACG, Mohammad Al-Haddad, MD, FACG
Indiana University School of Medicine, Indianapolis, IN
Introduction: Peroral endoscopic myotomy (POEM) has become the treatment of choice for achalasia. However, the impact of myotomy length on POEM outcomes remains unclear, with previous meta-analyses being primarily based on observational studies. To improve the quality of evidence, we performed a systematic review and meta-analysis of randomized controlled trials (RCTs) comparing the outcomes of short versus standard-length endoscopic myotomy in patients with achalasia.
Methods: We conducted a comprehensive search in PubMed, Embase, and Web of Science databases to identify all RCTs that compared POEM using short myotomy with standard myotomy. The primary outcomes were clinical success and post-operative gastroesophageal reflux disease (GERD). Clinical success was defined as a post-operative Eckardt score of ≤3. The secondary outcomes were procedural time, length of hospital stay, and intraprocedural complications. Pooled odds ratio (OR) and mean difference (MD) with the corresponding 95% confidence intervals (CIs) were calculated using a random-effect model. A p-value < 0.05 was considered statistically significant. The Comprehensive Meta-Analysis version 4 software (Biostat, Englewood, NJ, USA) was used for statistical analysis.
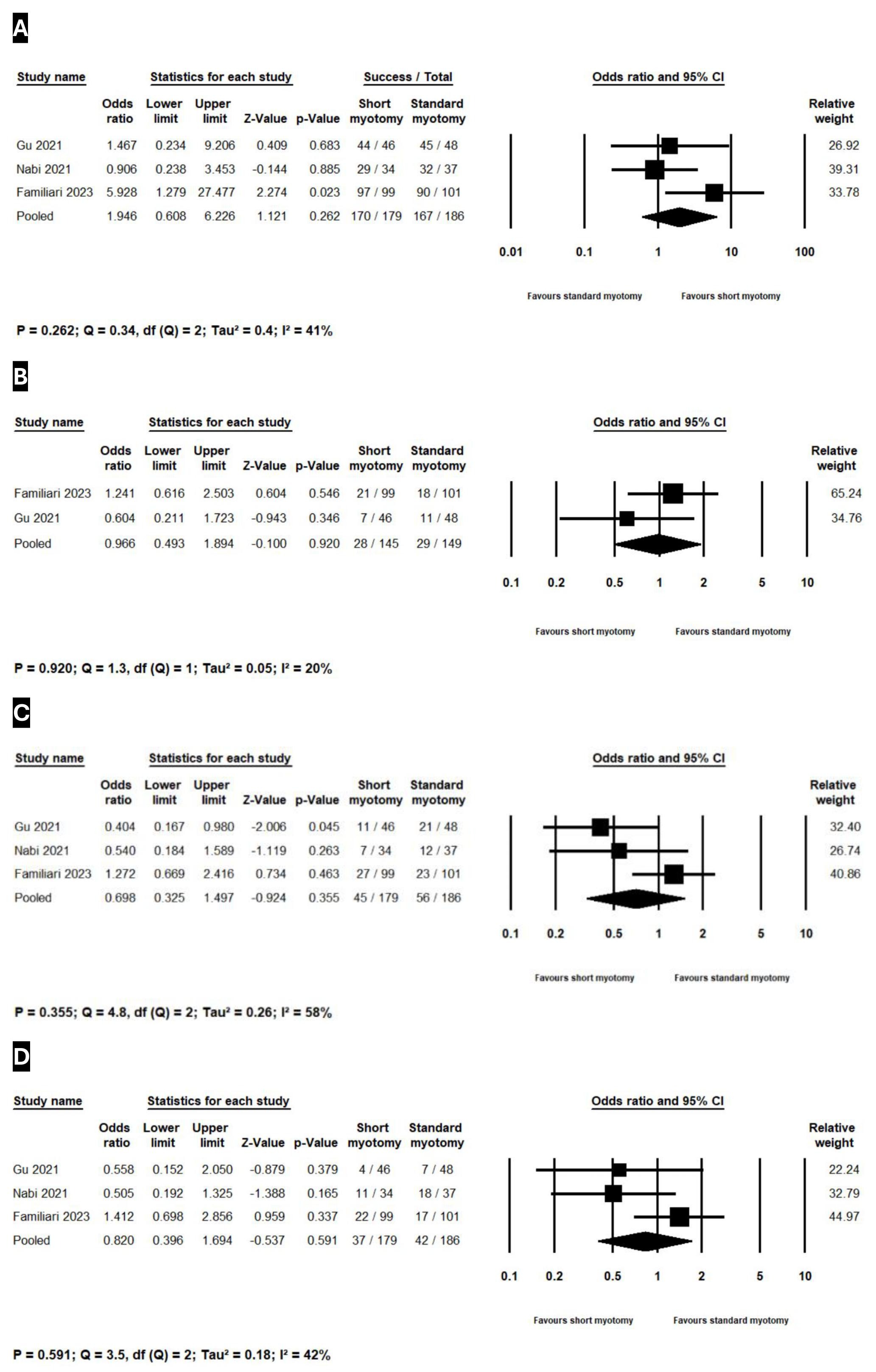
Results: Three RCTs with 365 achalasia patients treated with short (n=179) or standard (n=186) myotomy were included. Follow-up duration ranged from 12-24 months. The baseline study and patient characteristics of the included studies are summarized in Table 1. Short and standard myotomies showed similar clinical success (OR 1.95, 95% CI 0.61-6.23, p=0.26; I²=41%, Figure 1A), reflux symptoms (OR 0.97, 95% CI 0.49-1.89, p=0.92; I²=20%, Figure 1B), pathologic acid exposure on pH monitoring (OR 0.70, 95% CI 0.33-1.50, p=0.36; I²=58%, Figure 1C), reflux esophagitis on upper endoscopy (OR 0.82, 95% CI 0.40-1.70, p=0.59; I²=42%, Figure 1D), intraprocedural complications (OR 1.22, 95% CI 0.53-2.79, p=0.65; I²=0%), and length of hospital stay (MD -0.01, 95% CI -0.72 to 0.69, p=0.97, I²=73%). Procedural time was shorter in short myotomy (MD -16.11 mins, 95% CI -26.04 to -6.19, p=0.001; I²=84%).
Discussion: POEM using short myotomy for achalasia is non-inferior to standard myotomy for efficacy, safety, and post-operative GERD but is associated with a shorter procedural time. Further RCTs with longer follow-up data are needed to validate our findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Hashem Albunni, MD, Azizullah Beran, MD, Nwal Hadaki, MD, John M. DeWitt, MD, FACG, Mohammad Al-Haddad, MD, FACG. P4504 - Short Versus Standard Peroral Endoscopic Myotomy for Esophageal Achalasia: A Meta-Analysis of Randomized Controlled Trials, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Indiana University School of Medicine, Indianapolis, IN
Introduction: Peroral endoscopic myotomy (POEM) has become the treatment of choice for achalasia. However, the impact of myotomy length on POEM outcomes remains unclear, with previous meta-analyses being primarily based on observational studies. To improve the quality of evidence, we performed a systematic review and meta-analysis of randomized controlled trials (RCTs) comparing the outcomes of short versus standard-length endoscopic myotomy in patients with achalasia.
Methods: We conducted a comprehensive search in PubMed, Embase, and Web of Science databases to identify all RCTs that compared POEM using short myotomy with standard myotomy. The primary outcomes were clinical success and post-operative gastroesophageal reflux disease (GERD). Clinical success was defined as a post-operative Eckardt score of ≤3. The secondary outcomes were procedural time, length of hospital stay, and intraprocedural complications. Pooled odds ratio (OR) and mean difference (MD) with the corresponding 95% confidence intervals (CIs) were calculated using a random-effect model. A p-value < 0.05 was considered statistically significant. The Comprehensive Meta-Analysis version 4 software (Biostat, Englewood, NJ, USA) was used for statistical analysis.
Results: Three RCTs with 365 achalasia patients treated with short (n=179) or standard (n=186) myotomy were included. Follow-up duration ranged from 12-24 months. The baseline study and patient characteristics of the included studies are summarized in Table 1. Short and standard myotomies showed similar clinical success (OR 1.95, 95% CI 0.61-6.23, p=0.26; I²=41%, Figure 1A), reflux symptoms (OR 0.97, 95% CI 0.49-1.89, p=0.92; I²=20%, Figure 1B), pathologic acid exposure on pH monitoring (OR 0.70, 95% CI 0.33-1.50, p=0.36; I²=58%, Figure 1C), reflux esophagitis on upper endoscopy (OR 0.82, 95% CI 0.40-1.70, p=0.59; I²=42%, Figure 1D), intraprocedural complications (OR 1.22, 95% CI 0.53-2.79, p=0.65; I²=0%), and length of hospital stay (MD -0.01, 95% CI -0.72 to 0.69, p=0.97, I²=73%). Procedural time was shorter in short myotomy (MD -16.11 mins, 95% CI -26.04 to -6.19, p=0.001; I²=84%).
Discussion: POEM using short myotomy for achalasia is non-inferior to standard myotomy for efficacy, safety, and post-operative GERD but is associated with a shorter procedural time. Further RCTs with longer follow-up data are needed to validate our findings.
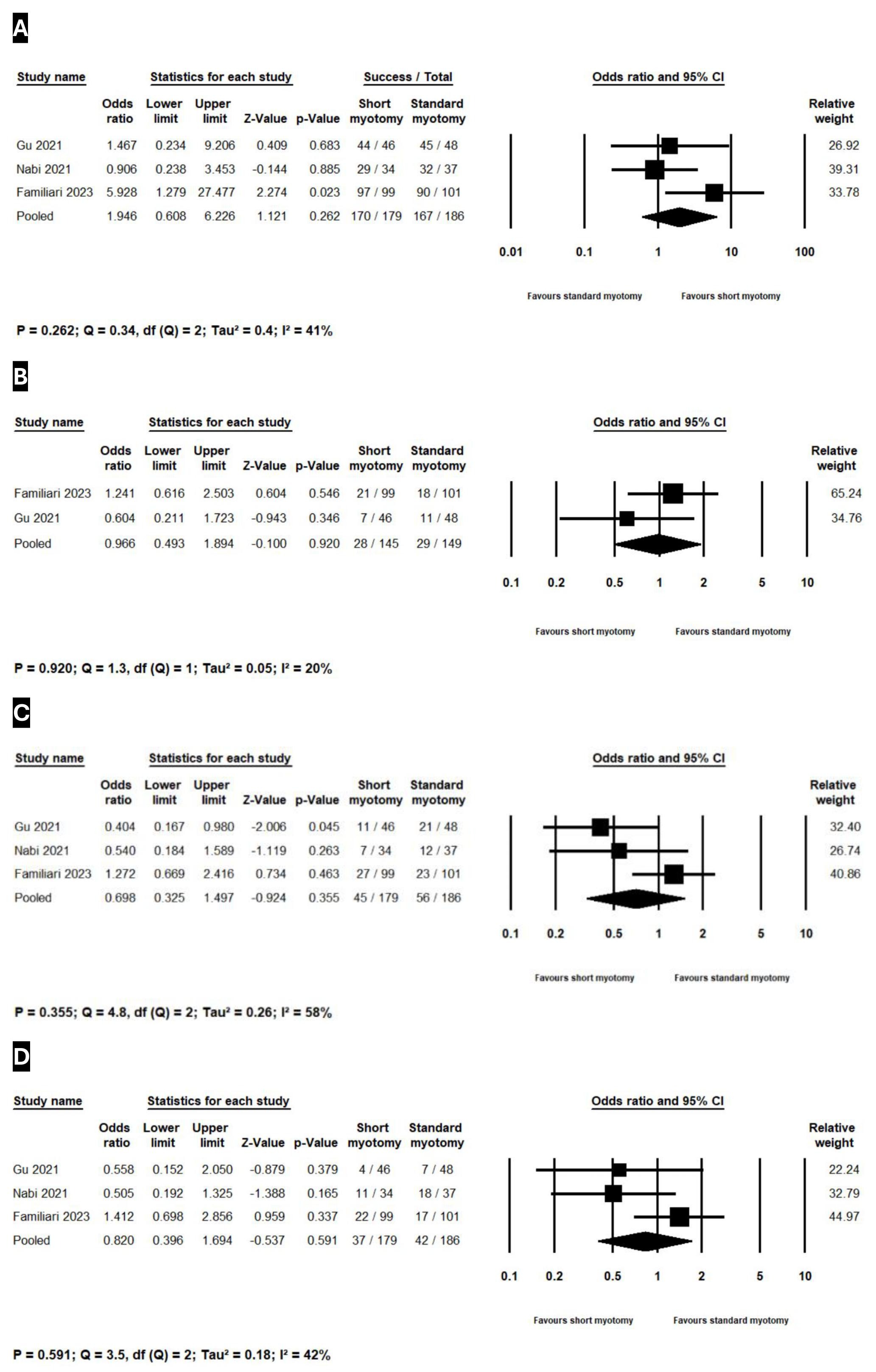
Figure: Figure 1. Forest plot showing the comparison of the primary outcomes in the short myotomy and the standard myotomy groups. (A) Clinical success. (B) Reflux symptoms. (C) Pathologic acid exposure on pH monitoring. (D) Reflux esophagitis on upper endoscopy
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Hashem Albunni indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Nwal Hadaki indicated no relevant financial relationships.
John DeWitt indicated no relevant financial relationships.
Mohammad Al-Haddad: Amplified Sciences – Grant/Research Support. Boston Scientific – Consultant. Interpace Diagnostics – Consultant.
Hashem Albunni, MD, Azizullah Beran, MD, Nwal Hadaki, MD, John M. DeWitt, MD, FACG, Mohammad Al-Haddad, MD, FACG. P4504 - Short Versus Standard Peroral Endoscopic Myotomy for Esophageal Achalasia: A Meta-Analysis of Randomized Controlled Trials, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

