Tuesday Poster Session
Category: Interventional Endoscopy
P4522 - Transoral Outlet Occlusion? An Adverse Event in Patients Undergoing Endoscopic Revision for Weight Regain After a Roux-en-Y Gastric Bypass (RYGB)
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Carter E. Edmunds, MD
University of Alabama at Birmingham Hospital
Birmingham, AL
Presenting Author(s)
Carter E. Edmunds, MD1, Babusai Rapaka, MD2, Ramzi Mulki, MD2, Sergio A. Sánchez-Luna, MD2
1University of Alabama at Birmingham Hospital, Birmingham, AL; 2Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Introduction: Transoral outlet reduction (TORe) is a minimally invasive procedure utilized in many patients experiencing weight regain after a Roux-en-Y gastric bypass (RYGB). Due to the intervention's safety profile and effectiveness as a surgical revision, it is becoming more commonly used in practice. However, complications from the procedure that necessitate further intervention can still occur.
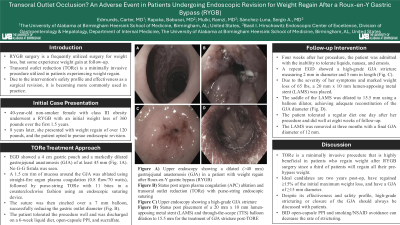
Case Description/Methods: A 40-year-old non-smoker female with class III obesity underwent a RYGB eight years prior with an initial weight loss of 360 pounds over the first 1.5 years. After this period, she experienced weight regain of over 120 pounds, and the patient opted to pursue endoscopic revision. Esophagogastroduodenoscopy (EGD) showed a 4 cm gastric pouch and a markedly dilated gastrojejunal anastomosis (GJA) of at least 45 mm (Fig. 1A). A 1.5 cm rim of mucosa around the GJA was ablated using straight fire argon plasma coagulation (APC, 0.8 flow, 70 Watts) followed by purse-string TORe with 11 bites using an endoscopic suturing device. The suture was then cinched over a 7 mm balloon, successfully reducing the gastric outlet size (Fig. 1B). The patient tolerated the procedure well and was discharged on a 6-week liquid diet, BID open-capsule proton-pump inhibitor (PPI) and QID carrafate. Four weeks after her procedure, the patient was admitted with the inability to tolerate liquids, nausea, and emesis. A repeat EGD showed a high-grade GJA stricture measuring 2 mm in diameter and 5 mm in length (Fig. 1C). Retained contents were seen in the pouch. Due to the severity of her symptoms and marked weight loss of 65 lbs, a 20 mm x 10 mm lumen-apposing metal stent (LAMS) was placed. The saddle of the LAMS was dilated to 15.5 mm using a balloon dilator, achieving adequate reconstitution of the GJA diameter (Fig. 1D). The patient tolerated a regular diet one day after her procedure and did well at eight weeks of follow-up.
Discussion: TORe is a minimally invasive procedure that is highly beneficial in patients who regain weight after RYGB surgery since a third of patients will regain all their pre-bypass weight. Ideal candidates are two years post-op, have regained ≥15% of the initial maximum weight loss, and have a GJA of ≥15 mm diameter. Despite its effectiveness and safety profile, high-grade stricturing or closure of the GJA should always be discussed with patients. BID open-capsule PPI and smoking/NSAID avoidance can decrease the rate of stricturing.

Disclosures:
Carter E. Edmunds, MD1, Babusai Rapaka, MD2, Ramzi Mulki, MD2, Sergio A. Sánchez-Luna, MD2. P4522 - Transoral Outlet Occlusion? An Adverse Event in Patients Undergoing Endoscopic Revision for Weight Regain After a Roux-en-Y Gastric Bypass (RYGB), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Alabama at Birmingham Hospital, Birmingham, AL; 2Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Introduction: Transoral outlet reduction (TORe) is a minimally invasive procedure utilized in many patients experiencing weight regain after a Roux-en-Y gastric bypass (RYGB). Due to the intervention's safety profile and effectiveness as a surgical revision, it is becoming more commonly used in practice. However, complications from the procedure that necessitate further intervention can still occur.
Case Description/Methods: A 40-year-old non-smoker female with class III obesity underwent a RYGB eight years prior with an initial weight loss of 360 pounds over the first 1.5 years. After this period, she experienced weight regain of over 120 pounds, and the patient opted to pursue endoscopic revision. Esophagogastroduodenoscopy (EGD) showed a 4 cm gastric pouch and a markedly dilated gastrojejunal anastomosis (GJA) of at least 45 mm (Fig. 1A). A 1.5 cm rim of mucosa around the GJA was ablated using straight fire argon plasma coagulation (APC, 0.8 flow, 70 Watts) followed by purse-string TORe with 11 bites using an endoscopic suturing device. The suture was then cinched over a 7 mm balloon, successfully reducing the gastric outlet size (Fig. 1B). The patient tolerated the procedure well and was discharged on a 6-week liquid diet, BID open-capsule proton-pump inhibitor (PPI) and QID carrafate. Four weeks after her procedure, the patient was admitted with the inability to tolerate liquids, nausea, and emesis. A repeat EGD showed a high-grade GJA stricture measuring 2 mm in diameter and 5 mm in length (Fig. 1C). Retained contents were seen in the pouch. Due to the severity of her symptoms and marked weight loss of 65 lbs, a 20 mm x 10 mm lumen-apposing metal stent (LAMS) was placed. The saddle of the LAMS was dilated to 15.5 mm using a balloon dilator, achieving adequate reconstitution of the GJA diameter (Fig. 1D). The patient tolerated a regular diet one day after her procedure and did well at eight weeks of follow-up.
Discussion: TORe is a minimally invasive procedure that is highly beneficial in patients who regain weight after RYGB surgery since a third of patients will regain all their pre-bypass weight. Ideal candidates are two years post-op, have regained ≥15% of the initial maximum weight loss, and have a GJA of ≥15 mm diameter. Despite its effectiveness and safety profile, high-grade stricturing or closure of the GJA should always be discussed with patients. BID open-capsule PPI and smoking/NSAID avoidance can decrease the rate of stricturing.

Figure: Figure 1. A) Upper endoscopy showing a dilated (>40 mm) gastrojejunal anastomosis (GJA) in a patient with weight regain after Roux-en-Y gastric bypass (RYGB); B) Status post argon plasma coagulation (APC) ablation and transoral outlet reduction (TORe) with purse-string endoscopic suturing; C) Upper endoscopy showing a high-grade GJA stricture; D) Status post placement of a 20 mm x 10 mm lumen-apposing metal stent (LAMS) and through-the-scope (TTS) balloon dilation to 15.5 mm for the treatment of GJA stricture post-TORE.
Disclosures:
Carter Edmunds indicated no relevant financial relationships.
Babusai Rapaka indicated no relevant financial relationships.
Ramzi Mulki indicated no relevant financial relationships.
Sergio A. Sánchez-Luna indicated no relevant financial relationships.
Carter E. Edmunds, MD1, Babusai Rapaka, MD2, Ramzi Mulki, MD2, Sergio A. Sánchez-Luna, MD2. P4522 - Transoral Outlet Occlusion? An Adverse Event in Patients Undergoing Endoscopic Revision for Weight Regain After a Roux-en-Y Gastric Bypass (RYGB), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

