Tuesday Poster Session
Category: Interventional Endoscopy
P4523 - Complex Endoscopic Management of Pancreatitis Complicated by Walled-Off Necrosis and Biliary Fistula
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Chineye Brenda Amuchi, MD, MPH
Beth Israel Lahey Health
Burlington, MA
Presenting Author(s)
Chineye Brenda Amuchi, MD, MPH1, Akshay Kapoor, MD2, Neethi Dasu, DO1, Mena Bakhit, MD2, Haider Rahman, MD2, Khaldoon Khirfan, MD1
1Beth Israel Lahey Health, Burlington, MA; 2Lahey Hospital and Medical Center, Burlington, MA
Introduction: Pancreatitis complications, such as walled-off necrosis (WON) and biliary fistulas, pose significant treatment challenges. This case presents a complex scenario involving a middle-aged man who developed WON and biliary fistulas following ampullectomy. It emphasizes the successful endoscopic management of pancreatic WON and associated fistulae.
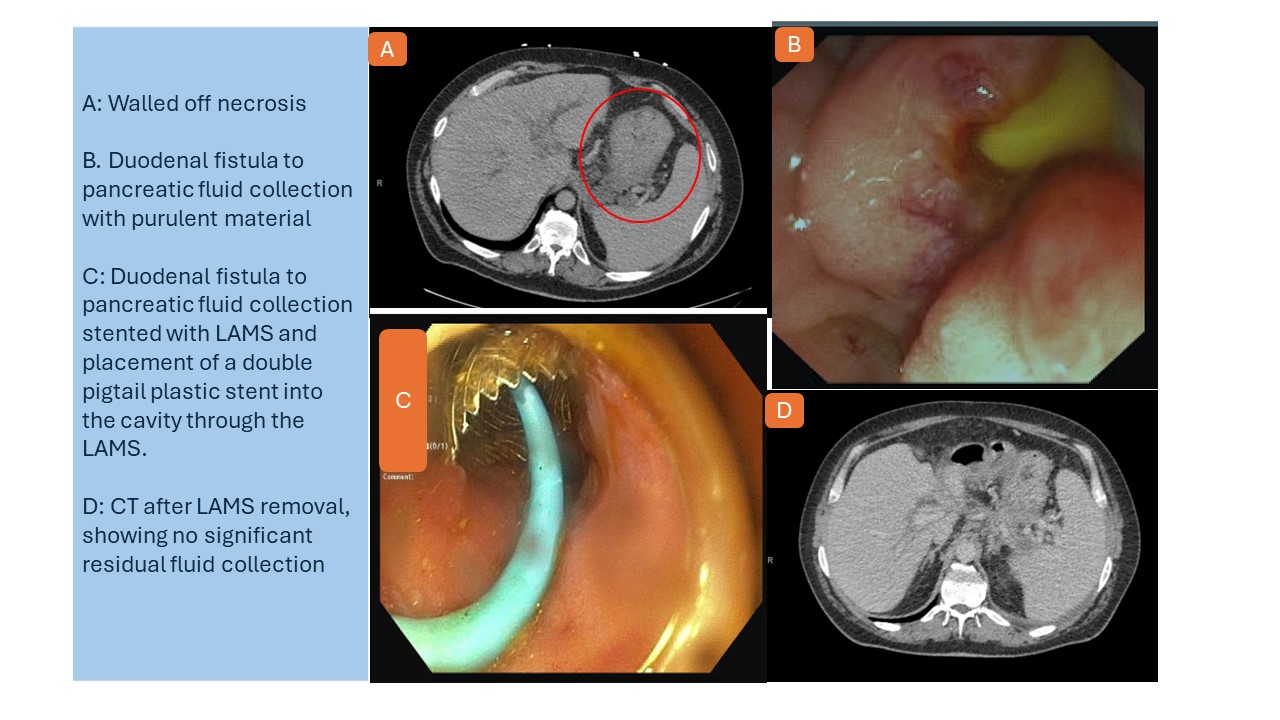
Case Description/Methods: A 48-year-old man with a history of gastroesophageal reflux disease (GERD) underwent routine esophagogastroduodenoscopy (EGD) for long-standing GERD. He was found to have a 3 cm ampullary adenoma and underwent endoscopic ultrasound-guided endoscopic retrograde cholangiopancreatography (EUS-ERCP) and endoscopic mucosal resection of the ampullary adenoma. Despite the successful closure of the peri-ampullary defect with clips, attempts to cannulate the pancreatic duct were unsuccessful due to unclear landmarks post-resection. Post-procedure, he developed worsening abdominal pain and a lipase of 14,000 u/l. A CT scan revealed acute interstitial pancreatitis.
Given persistent symptoms, a repeat CT scan indicated necrotizing pancreatitis without walled-off necrosis initially, but subsequent imaging revealed extensive pancreatic and peripancreatic necrosis with gas and a loculated fluid collection in the lesser sac. Endoscopic procedures identified a duodenal bulb-to-collection fistula and a common hepatic duct (CHD)-to-collection fistula. Staged endoscopic management included placement of fully covered self-expanding metal stents (FCSEMS) in the bile duct, placement of lumen-apposing metal stent (LAMS) creating a cystoduodenostomy and insertion of two double pigtail stents into the duodenal bulb collection. Follow-up ERCP confirmed the resolution of the biliary fistula and improved WON, allowing for the removal of metal stents and insertion of permanent double pigtail stent into the residual WON. Recent CT imaging verified the complete resolution of WON.
Discussion: Managing post-pancreatitis peri-pancreatic fluid collections, especially WON with associated fistulas, presents significant challenges. This case underscores the evolving role of endoscopy as a minimally invasive alternative to surgery in treating severe pancreatitis sequelae. We showcase the utilization of three distinct endoscopic techniques that effectively address fistulas related to WON. This approach reduces the need for surgical interventions and improves recovery times.
Disclosures:
Chineye Brenda Amuchi, MD, MPH1, Akshay Kapoor, MD2, Neethi Dasu, DO1, Mena Bakhit, MD2, Haider Rahman, MD2, Khaldoon Khirfan, MD1. P4523 - Complex Endoscopic Management of Pancreatitis Complicated by Walled-Off Necrosis and Biliary Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Beth Israel Lahey Health, Burlington, MA; 2Lahey Hospital and Medical Center, Burlington, MA
Introduction: Pancreatitis complications, such as walled-off necrosis (WON) and biliary fistulas, pose significant treatment challenges. This case presents a complex scenario involving a middle-aged man who developed WON and biliary fistulas following ampullectomy. It emphasizes the successful endoscopic management of pancreatic WON and associated fistulae.
Case Description/Methods: A 48-year-old man with a history of gastroesophageal reflux disease (GERD) underwent routine esophagogastroduodenoscopy (EGD) for long-standing GERD. He was found to have a 3 cm ampullary adenoma and underwent endoscopic ultrasound-guided endoscopic retrograde cholangiopancreatography (EUS-ERCP) and endoscopic mucosal resection of the ampullary adenoma. Despite the successful closure of the peri-ampullary defect with clips, attempts to cannulate the pancreatic duct were unsuccessful due to unclear landmarks post-resection. Post-procedure, he developed worsening abdominal pain and a lipase of 14,000 u/l. A CT scan revealed acute interstitial pancreatitis.
Given persistent symptoms, a repeat CT scan indicated necrotizing pancreatitis without walled-off necrosis initially, but subsequent imaging revealed extensive pancreatic and peripancreatic necrosis with gas and a loculated fluid collection in the lesser sac. Endoscopic procedures identified a duodenal bulb-to-collection fistula and a common hepatic duct (CHD)-to-collection fistula. Staged endoscopic management included placement of fully covered self-expanding metal stents (FCSEMS) in the bile duct, placement of lumen-apposing metal stent (LAMS) creating a cystoduodenostomy and insertion of two double pigtail stents into the duodenal bulb collection. Follow-up ERCP confirmed the resolution of the biliary fistula and improved WON, allowing for the removal of metal stents and insertion of permanent double pigtail stent into the residual WON. Recent CT imaging verified the complete resolution of WON.
Discussion: Managing post-pancreatitis peri-pancreatic fluid collections, especially WON with associated fistulas, presents significant challenges. This case underscores the evolving role of endoscopy as a minimally invasive alternative to surgery in treating severe pancreatitis sequelae. We showcase the utilization of three distinct endoscopic techniques that effectively address fistulas related to WON. This approach reduces the need for surgical interventions and improves recovery times.
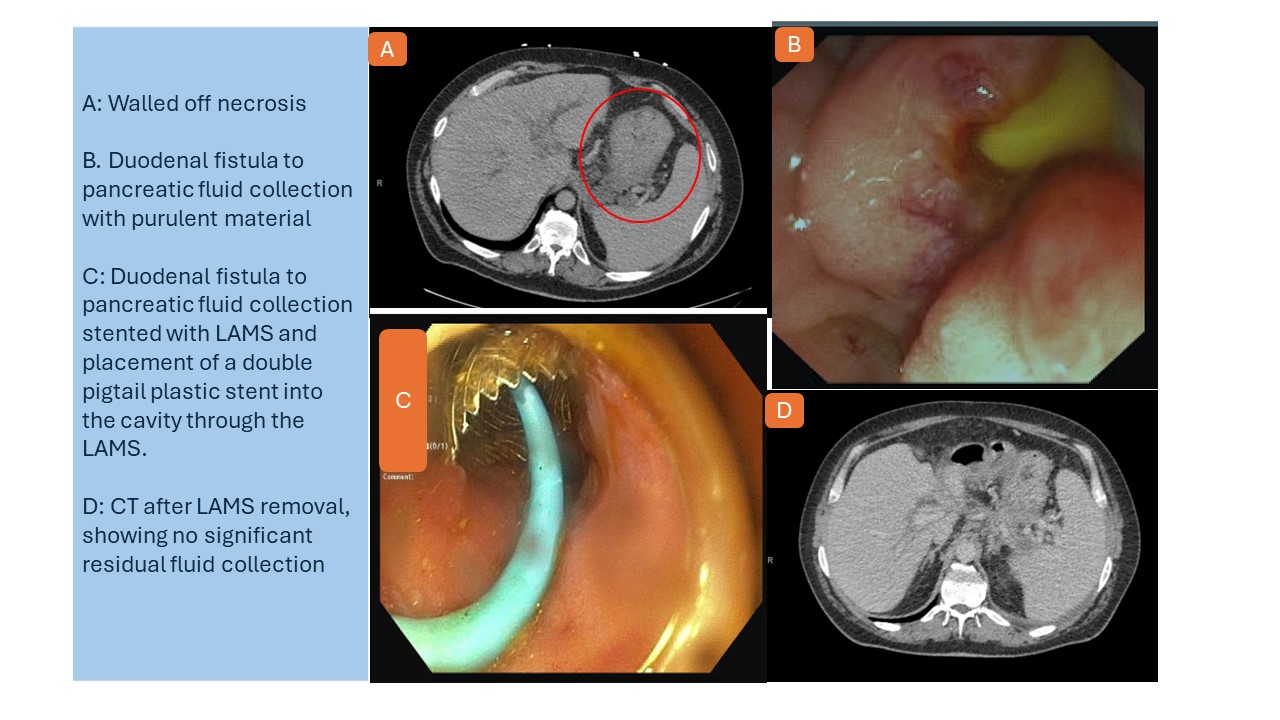
Figure: CT and Endoscopy Images
Disclosures:
Chineye Brenda Amuchi indicated no relevant financial relationships.
Akshay Kapoor indicated no relevant financial relationships.
Neethi Dasu indicated no relevant financial relationships.
Mena Bakhit indicated no relevant financial relationships.
Haider Rahman indicated no relevant financial relationships.
Khaldoon Khirfan indicated no relevant financial relationships.
Chineye Brenda Amuchi, MD, MPH1, Akshay Kapoor, MD2, Neethi Dasu, DO1, Mena Bakhit, MD2, Haider Rahman, MD2, Khaldoon Khirfan, MD1. P4523 - Complex Endoscopic Management of Pancreatitis Complicated by Walled-Off Necrosis and Biliary Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
