Tuesday Poster Session
Category: IBD
P4432 - Recurrent Splenic Abscesses in a Patient With Ulcerative Colitis and Pouchitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Inas FS Fouad Soliman Mikhail, MD, MSc
Mayo Clinic
Jacksonville, Egypt
Presenting Author(s)
Inas FS. Fouad Soliman Mikhail, MD, MSc, Tarek Odah, MD, Katherine Poruk, MD, Justin M. Oring, DO, Francis A. Farraye, MD, MSc, Jana G. Hashash, MD, MSc
Mayo Clinic, Jacksonville, FL
Introduction: Splenic abscesses, often from bacteremia or direct extension, typically cause fever, left upper quadrant pain, and leukocytosis, with infective endocarditis as a common cause. Despite treatment, mortality can approach 70%. Ulcerative colitis (UC), heightens infection susceptibility due to elevated inflammatory cytokines and immune-thrombosis, potentially leading to bacteremia, splenic thrombosis, and infarctions. Severe pouchitis further compromises the mucosal intestinal barrier, increasing bacterial translocation risk. Here, we present a case of recurrent splenic abscesses in a patient with pouchitis.
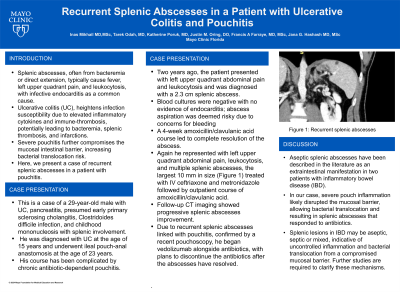
Case Description/Methods: This is a case of a 29-year-old male with UC, pancreatitis, presumed early primary sclerosing cholangitis, Clostridoides difficile infection, and childhood mononucleosis with splenic involvement. He was diagnosed with UC at age 15 years and underwent ileal pouch anal anastomosis at age 23 years. His course has been complicated by chronic antibiotic dependent pouchitis. Two years ago, the patient presented with left upper quadrant abdominal pain and leukocytosis and was diagnosed with a 2.3 cm splenic abscess. Blood cultures were negative with no evidence of endocarditis; abscess aspiration was deemed risky due to concerns for bleeding. A 4-week course of amoxicillin/clavulanic acid led to complete resolution the abscess. He represented with left upper quadrant abdominal pain, leukocytosis, and multiple splenic abscesses, largest 10 mm in size (Figure 1) treated with IV ceftriaxone and metronidazole followed by outpatient course of amoxicillin/clavulanic acid. Follow-up CT imaging showed progressive splenic abscesses improvement. Due to recurrent splenic abscesses linked with pouchitis, confirmed by recent pouchoscopy, he began vedolizumab alongside antibiotics, with plans to discontinue the antibiotics after the abscesses have resolved.
Discussion: Aseptic splenic abscesses have been described in the literature as an extraintestinal manifestations in two patients with inflammatory bowel disease (IBD). In our case, severe pouch inflammation likely disrupted the mucosal barrier, allowing bacterial translocation and resulting in splenic abscesses that responded to antibiotics. This underscores that splenic lesions in IBD may be aseptic, septic or mixed, indicative of uncontrolled inflammation and bacterial translocation from a compromised mucosal barrier. Further studies are required to clarify these mechanisms.

Disclosures:
Inas FS. Fouad Soliman Mikhail, MD, MSc, Tarek Odah, MD, Katherine Poruk, MD, Justin M. Oring, DO, Francis A. Farraye, MD, MSc, Jana G. Hashash, MD, MSc. P4432 - Recurrent Splenic Abscesses in a Patient With Ulcerative Colitis and Pouchitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Jacksonville, FL
Introduction: Splenic abscesses, often from bacteremia or direct extension, typically cause fever, left upper quadrant pain, and leukocytosis, with infective endocarditis as a common cause. Despite treatment, mortality can approach 70%. Ulcerative colitis (UC), heightens infection susceptibility due to elevated inflammatory cytokines and immune-thrombosis, potentially leading to bacteremia, splenic thrombosis, and infarctions. Severe pouchitis further compromises the mucosal intestinal barrier, increasing bacterial translocation risk. Here, we present a case of recurrent splenic abscesses in a patient with pouchitis.
Case Description/Methods: This is a case of a 29-year-old male with UC, pancreatitis, presumed early primary sclerosing cholangitis, Clostridoides difficile infection, and childhood mononucleosis with splenic involvement. He was diagnosed with UC at age 15 years and underwent ileal pouch anal anastomosis at age 23 years. His course has been complicated by chronic antibiotic dependent pouchitis. Two years ago, the patient presented with left upper quadrant abdominal pain and leukocytosis and was diagnosed with a 2.3 cm splenic abscess. Blood cultures were negative with no evidence of endocarditis; abscess aspiration was deemed risky due to concerns for bleeding. A 4-week course of amoxicillin/clavulanic acid led to complete resolution the abscess. He represented with left upper quadrant abdominal pain, leukocytosis, and multiple splenic abscesses, largest 10 mm in size (Figure 1) treated with IV ceftriaxone and metronidazole followed by outpatient course of amoxicillin/clavulanic acid. Follow-up CT imaging showed progressive splenic abscesses improvement. Due to recurrent splenic abscesses linked with pouchitis, confirmed by recent pouchoscopy, he began vedolizumab alongside antibiotics, with plans to discontinue the antibiotics after the abscesses have resolved.
Discussion: Aseptic splenic abscesses have been described in the literature as an extraintestinal manifestations in two patients with inflammatory bowel disease (IBD). In our case, severe pouch inflammation likely disrupted the mucosal barrier, allowing bacterial translocation and resulting in splenic abscesses that responded to antibiotics. This underscores that splenic lesions in IBD may be aseptic, septic or mixed, indicative of uncontrolled inflammation and bacterial translocation from a compromised mucosal barrier. Further studies are required to clarify these mechanisms.

Figure: Figure 1: Recurrent splenic abscesses
Disclosures:
Inas Fouad Soliman Mikhail indicated no relevant financial relationships.
Tarek Odah indicated no relevant financial relationships.
Katherine Poruk indicated no relevant financial relationships.
Justin M. Oring indicated no relevant financial relationships.
Francis Farraye: AbbVie – Consultant. Avalo Therapeutics – Consultant. Bausch – Advisor or Review Panel Member. BMS – Consultant. Braintree Labs – Consultant. DSMB for Lilly. – Sits on. Fresenius Kabi – Consultant. GI Reviewers and IBD Educational Group – independent contractor. GSK, Iterative Health, Janssen, Pfizer, Pharmacosmos, Sandoz Immunology, Sebela and Viatris – Consultant.
Jana Hashash: Bristol Myers Squibb – Consultant.
Inas FS. Fouad Soliman Mikhail, MD, MSc, Tarek Odah, MD, Katherine Poruk, MD, Justin M. Oring, DO, Francis A. Farraye, MD, MSc, Jana G. Hashash, MD, MSc. P4432 - Recurrent Splenic Abscesses in a Patient With Ulcerative Colitis and Pouchitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
