Tuesday Poster Session
Category: IBD
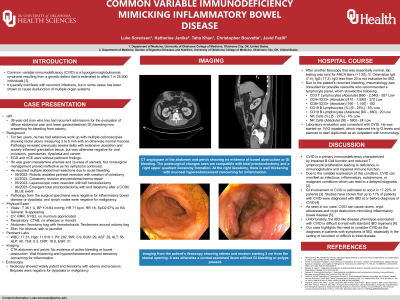
P4434 - Common Variable Immunodeficiency Mimicking Inflammatory Bowel Disease
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Luke Sorensen, MD
University of Oklahoma Health Sciences Center
Oklahoma City, OK
Presenting Author(s)
Luke Sorensen, MD1, Katherine Janike, MD2, Taha Khan, MD1, Christopher Bouvette, MD1, Javid Fazili, MD1
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2University of Oklahoma College of Medicine, Oklahoma City, OK
Introduction: Common variable immunodeficiency (CVID) is a hypogammaglobulinemia syndrome resulting from a genetic defect that is estimated to affect 1 in 25,000 individuals [1]. It typically manifests with recurrent infections, but in some cases has been shown to cause dysfunction of multiple organ systems.
Case Description/Methods: We present a 38-year-old man who has had recurrent admissions for the evaluation of lower gastrointestinal (GI) bleeding. For two years, he has had extensive work up with multiple colonoscopies, EGDs and VCEs that were unremarkable apart from rectal ulcers measuring 3 to 5 mm. Pathology revealed mild cryptitis and negative CMV viral titers. He was given mesalamine enemas and steroids, but his symptoms continued. Nonsurgical management proved ineffective, and he required an abdominal perineal resection to stabilize an episode of hemorrhagic shock. At a future hospital admission, an endoscopy revealed ulcerated mucosa at the surgical stoma, a peristomal hernia, and a peristomal perforation requiring a stoma takedown. He continued to have recurrent episodes of bleeding secondary to ulceration and ultimately required a total colectomy. Pathology from this surgical specimen was negative for inflammatory bowel disease, dysplasia, and malignancy. Further workup was obtained and revealed a reduced IgG level at 288 with a lymphocyte panel exhibiting decreased absolute CD3 T lymphocytes, CD19 B lymphocytes and NK cells consistent with CVID. The patient is currently being managed with IVIG and dupilumab as an outpatient.
Discussion: CVID is a primary immunodeficiency characterized by impaired B Cell function and reduced T lymphocyte proliferation leading to deficiency in immunoglobulins and impaired immune function. Due to the variable expression of this condition, CVID can manifest as infectious, inflammatory, autoimmune, or malignant conditions which can lead to a delayed diagnosis [2]. GI involvement of CVID is estimated to occur in 17-22% of patients [3]. Studies have shown that up to 11% of patients with CVID were diagnosed with IBD at or before diagnosis of CVID [4]. As seen in our case, CVID can cause ulcers, crypt abscesses and crypt destruction mimicking inflammatory bowel disease [5]. Unfortunately, the IBD-like disease phenotype associated with CVID is difficult to treat with standard IBD regimens [6]. Our case highlights the need to consider CVID as the diagnosis in patients with symptoms of IBD, especially in the setting of recurrent or difficult to treat disease.
Disclosures:
Luke Sorensen, MD1, Katherine Janike, MD2, Taha Khan, MD1, Christopher Bouvette, MD1, Javid Fazili, MD1. P4434 - Common Variable Immunodeficiency Mimicking Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2University of Oklahoma College of Medicine, Oklahoma City, OK
Introduction: Common variable immunodeficiency (CVID) is a hypogammaglobulinemia syndrome resulting from a genetic defect that is estimated to affect 1 in 25,000 individuals [1]. It typically manifests with recurrent infections, but in some cases has been shown to cause dysfunction of multiple organ systems.
Case Description/Methods: We present a 38-year-old man who has had recurrent admissions for the evaluation of lower gastrointestinal (GI) bleeding. For two years, he has had extensive work up with multiple colonoscopies, EGDs and VCEs that were unremarkable apart from rectal ulcers measuring 3 to 5 mm. Pathology revealed mild cryptitis and negative CMV viral titers. He was given mesalamine enemas and steroids, but his symptoms continued. Nonsurgical management proved ineffective, and he required an abdominal perineal resection to stabilize an episode of hemorrhagic shock. At a future hospital admission, an endoscopy revealed ulcerated mucosa at the surgical stoma, a peristomal hernia, and a peristomal perforation requiring a stoma takedown. He continued to have recurrent episodes of bleeding secondary to ulceration and ultimately required a total colectomy. Pathology from this surgical specimen was negative for inflammatory bowel disease, dysplasia, and malignancy. Further workup was obtained and revealed a reduced IgG level at 288 with a lymphocyte panel exhibiting decreased absolute CD3 T lymphocytes, CD19 B lymphocytes and NK cells consistent with CVID. The patient is currently being managed with IVIG and dupilumab as an outpatient.
Discussion: CVID is a primary immunodeficiency characterized by impaired B Cell function and reduced T lymphocyte proliferation leading to deficiency in immunoglobulins and impaired immune function. Due to the variable expression of this condition, CVID can manifest as infectious, inflammatory, autoimmune, or malignant conditions which can lead to a delayed diagnosis [2]. GI involvement of CVID is estimated to occur in 17-22% of patients [3]. Studies have shown that up to 11% of patients with CVID were diagnosed with IBD at or before diagnosis of CVID [4]. As seen in our case, CVID can cause ulcers, crypt abscesses and crypt destruction mimicking inflammatory bowel disease [5]. Unfortunately, the IBD-like disease phenotype associated with CVID is difficult to treat with standard IBD regimens [6]. Our case highlights the need to consider CVID as the diagnosis in patients with symptoms of IBD, especially in the setting of recurrent or difficult to treat disease.
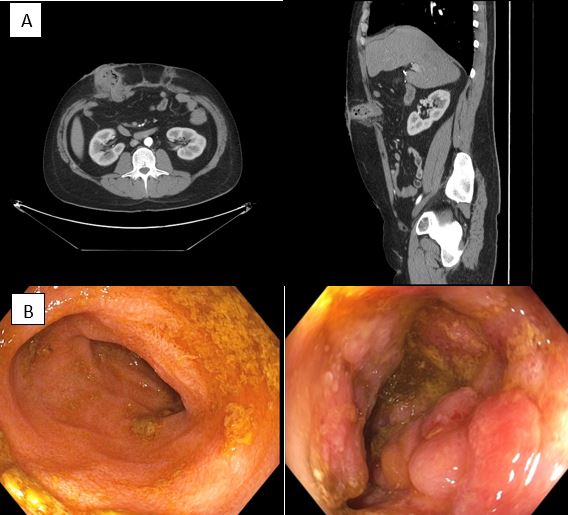
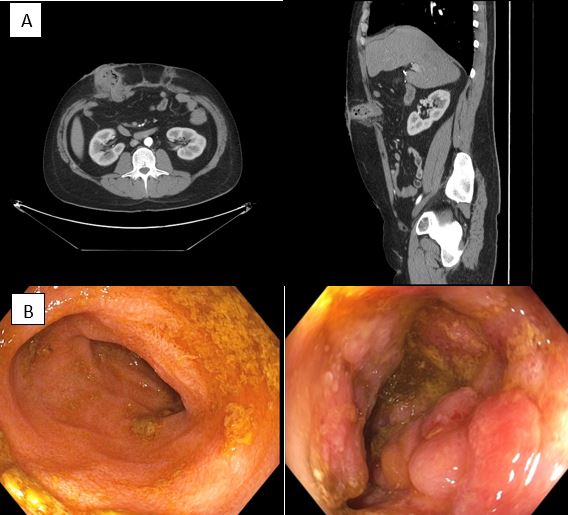
Figure: A) CT angiogram of the abdomen and pelvis showing no evidence of bowel obstruction or GI bleeding. The postsurgical changes seen are compatible with total proctocolectomy and a right upper quadrant ileostomy formation. At the right ileostomy, there is wall thickening with mucosal hyperenhancement concerning for inflammation.
B) Imaging from the patient’s ileoscopy showing edema and erosion starting 2 cm from the stomal opening. It was otherwise a normal examined ileum without GI bleeding or polyps present.
B) Imaging from the patient’s ileoscopy showing edema and erosion starting 2 cm from the stomal opening. It was otherwise a normal examined ileum without GI bleeding or polyps present.
Disclosures:
Luke Sorensen indicated no relevant financial relationships.
Katherine Janike indicated no relevant financial relationships.
Taha Khan indicated no relevant financial relationships.
Christopher Bouvette indicated no relevant financial relationships.
Javid Fazili indicated no relevant financial relationships.
Luke Sorensen, MD1, Katherine Janike, MD2, Taha Khan, MD1, Christopher Bouvette, MD1, Javid Fazili, MD1. P4434 - Common Variable Immunodeficiency Mimicking Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
