Tuesday Poster Session
Category: IBD
P4349 - Let’s Talk About It: The Mysterious Silence of IBD Patients in a Community Primary Care Clinic
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Advait Suvarnakar, BS
MedStar Georgetown University Hospital
Washington, DC
Presenting Author(s)
Advait Suvarnakar, BS1, Faisal Nagarwala, MD2
1MedStar Georgetown University Hospital, Washington, DC; 2St. Joseph's University Medical Center, Clifton, NJ
Introduction: Patient disclosure to clinicians is fundamental for effective clinician-patient relationships and quality patient care. Clinicians depend on patients to disclose symptoms, health behaviors, and thoughts for accurate diagnoses and treatment recommendations. In general practice, gastrointestinal (GI) disorders are prevalent, constituting approximately 10% of general practitioners' workload. Irritable bowel disease (IBD), diagnosable by gastroenterologists, often necessitates long-term monitoring, which primary care physicians (PCPs) can undertake, given their frequent patient interactions. This study aims to investigate why newly diagnosed IBD patients at a single community care site often fail to disclose their diagnosis during initial consultations.
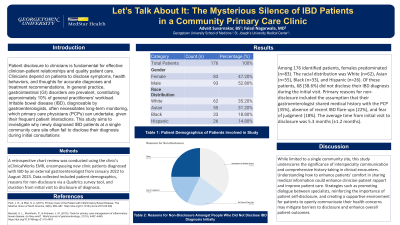
Methods: A retrospective chart review was conducted using the clinic's eClinicalWorks EMR, encompassing new clinic patients diagnosed with IBD by an external gastroenterologist from January 2022 to August 2023. Data collected included patient demographics, reasons for non-disclosure via a Qualtrics survey tool, and duration from initial visit to disclosure of diagnosis.
Results: Among 176 identified patients, females predominated (n=83). The racial distribution was White (n=62), Asian (n=55), Black (n=33), and Hispanic (n=26). Of these patients, 68 (38.6%) did not disclose their IBD diagnosis during the initial visit. Primary reasons for non-disclosure included the assumption that their gastroenterologist shared medical history with the PCP (35%), absence of recent IBD flare-ups (22%), and fear of judgment (18%). The average time from initial visit to disclosure was 5.3 months (±1.2 months).
Discussion: While limited to a single community site, this study underscores the significance of interspecialty communication and comprehensive history-taking in clinical encounters. Understanding how to enhance patients' comfort in sharing medical information could enhance clinician-patient rapport and improve patient care. Strategies such as promoting dialogue between specialists, reinforcing the importance of patient self-disclosure, and creating a supportive environment for patients to openly communicate their health concerns may mitigate barriers to disclosure and enhance overall patient outcomes.
Disclosures:
Advait Suvarnakar, BS1, Faisal Nagarwala, MD2. P4349 - Let’s Talk About It: The Mysterious Silence of IBD Patients in a Community Primary Care Clinic, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1MedStar Georgetown University Hospital, Washington, DC; 2St. Joseph's University Medical Center, Clifton, NJ
Introduction: Patient disclosure to clinicians is fundamental for effective clinician-patient relationships and quality patient care. Clinicians depend on patients to disclose symptoms, health behaviors, and thoughts for accurate diagnoses and treatment recommendations. In general practice, gastrointestinal (GI) disorders are prevalent, constituting approximately 10% of general practitioners' workload. Irritable bowel disease (IBD), diagnosable by gastroenterologists, often necessitates long-term monitoring, which primary care physicians (PCPs) can undertake, given their frequent patient interactions. This study aims to investigate why newly diagnosed IBD patients at a single community care site often fail to disclose their diagnosis during initial consultations.
Methods: A retrospective chart review was conducted using the clinic's eClinicalWorks EMR, encompassing new clinic patients diagnosed with IBD by an external gastroenterologist from January 2022 to August 2023. Data collected included patient demographics, reasons for non-disclosure via a Qualtrics survey tool, and duration from initial visit to disclosure of diagnosis.
Results: Among 176 identified patients, females predominated (n=83). The racial distribution was White (n=62), Asian (n=55), Black (n=33), and Hispanic (n=26). Of these patients, 68 (38.6%) did not disclose their IBD diagnosis during the initial visit. Primary reasons for non-disclosure included the assumption that their gastroenterologist shared medical history with the PCP (35%), absence of recent IBD flare-ups (22%), and fear of judgment (18%). The average time from initial visit to disclosure was 5.3 months (±1.2 months).
Discussion: While limited to a single community site, this study underscores the significance of interspecialty communication and comprehensive history-taking in clinical encounters. Understanding how to enhance patients' comfort in sharing medical information could enhance clinician-patient rapport and improve patient care. Strategies such as promoting dialogue between specialists, reinforcing the importance of patient self-disclosure, and creating a supportive environment for patients to openly communicate their health concerns may mitigate barriers to disclosure and enhance overall patient outcomes.
Disclosures:
Advait Suvarnakar indicated no relevant financial relationships.
Faisal Nagarwala indicated no relevant financial relationships.
Advait Suvarnakar, BS1, Faisal Nagarwala, MD2. P4349 - Let’s Talk About It: The Mysterious Silence of IBD Patients in a Community Primary Care Clinic, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
