Tuesday Poster Session
Category: GI Bleeding
P4249 - Fistula Formation Between Small Bowel and Pseudoaneurysm as a Source of an Upper Gastrointestinal Bleed
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio

Rhea Fogla, MD
New York-Presbyterian / Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Rhea Fogla, MD, Eliza Cricco-Lizza, MD, Carl V. Crawford, MD
New York-Presbyterian / Weill Cornell Medical Center, New York, NY
Introduction: Common etiologies of UGIB include peptic ulcer disease, esophagitis, gastritis, Mallory Weiss tear, angiodysplasia, and malignancy. Endoscopic evaluation is standard practice to identify the etiology, as well as provide therapeutic intervention. Here we present a case of UGIB that was secondary to fistula formation between a pseudoaneurysm and the small bowel.
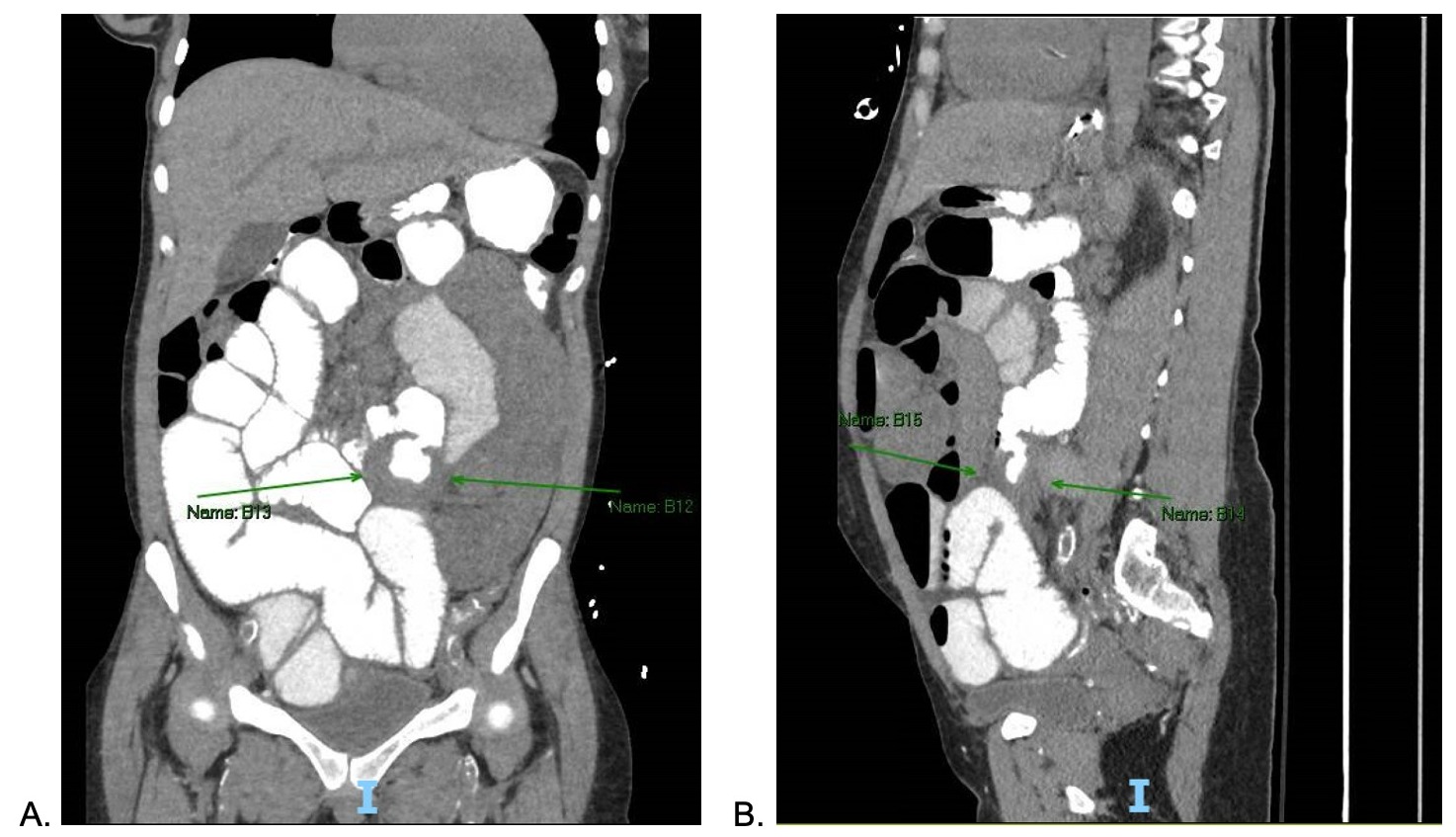
Case Description/Methods: A 39-year-old female with a history of type 1 diabetes mellitus, hypertension, and end stage renal disease status post simultaneous pancreas/kidney transplant presented to the hospital after a syncopal event with hematemesis and melena. Labs were notable for hemoglobin of 5.7 g/dL. CT Angiography Abdomen and Pelvis demonstrated a 7.8 x 5 cm pseudoaneurysm arising from the left common iliac artery and left renal artery stenosis, for which the patient underwent stent placement on the day of admission. Upper endoscopy and colonoscopy did not reveal an identifiable source of bleeding for her melena. She was planned for video capsule endoscopy (VCE) for further evaluation; however, she developed a new acute small bowel obstruction. Ten days later, the patient developed recurrent hematemesis and repeat abdominal imaging with PO contrast revealed a fistula between the small bowel and the pseudoaneurysm with enteric contrast extending into pseudoaneurysm. The patient underwent an exploratory laparotomy, which identified multiple adhesions and a fistula 30 cm from the ligament of Treitz. The surgery resulted in a small bowel resection with a primary end-to-end anastomosis, and washout, drainage, and resection of the pseudoaneurysm sac. The patient ultimately recovered and was discharged.
Discussion: This case illustrates fistula development as a rare cause of UGIB and highlights the multidisciplinary management of gastrointestinal bleeding in the setting of a negative endoscopic evaluation. VCE is increasingly utilized to investigate small bowel bleeds; however, one must be cautious with this approach, particularly in patients predisposed to adhesions or strictures due to history of major abdominal surgeries or chronic inflammatory states (i.e., Crohn’s). Recognizing factors contributing to pseudoaneurysm formation (i.e., trauma, infection, procedures with vascular manipulation), and therefore potential fistula development, is critical for guiding timely appropriate imaging and surgical involvement, as demonstrated in this case with focused imaging that prompted an operative intervention.
Disclosures:
Rhea Fogla, MD, Eliza Cricco-Lizza, MD, Carl V. Crawford, MD. P4249 - Fistula Formation Between Small Bowel and Pseudoaneurysm as a Source of an Upper Gastrointestinal Bleed, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
New York-Presbyterian / Weill Cornell Medical Center, New York, NY
Introduction: Common etiologies of UGIB include peptic ulcer disease, esophagitis, gastritis, Mallory Weiss tear, angiodysplasia, and malignancy. Endoscopic evaluation is standard practice to identify the etiology, as well as provide therapeutic intervention. Here we present a case of UGIB that was secondary to fistula formation between a pseudoaneurysm and the small bowel.
Case Description/Methods: A 39-year-old female with a history of type 1 diabetes mellitus, hypertension, and end stage renal disease status post simultaneous pancreas/kidney transplant presented to the hospital after a syncopal event with hematemesis and melena. Labs were notable for hemoglobin of 5.7 g/dL. CT Angiography Abdomen and Pelvis demonstrated a 7.8 x 5 cm pseudoaneurysm arising from the left common iliac artery and left renal artery stenosis, for which the patient underwent stent placement on the day of admission. Upper endoscopy and colonoscopy did not reveal an identifiable source of bleeding for her melena. She was planned for video capsule endoscopy (VCE) for further evaluation; however, she developed a new acute small bowel obstruction. Ten days later, the patient developed recurrent hematemesis and repeat abdominal imaging with PO contrast revealed a fistula between the small bowel and the pseudoaneurysm with enteric contrast extending into pseudoaneurysm. The patient underwent an exploratory laparotomy, which identified multiple adhesions and a fistula 30 cm from the ligament of Treitz. The surgery resulted in a small bowel resection with a primary end-to-end anastomosis, and washout, drainage, and resection of the pseudoaneurysm sac. The patient ultimately recovered and was discharged.
Discussion: This case illustrates fistula development as a rare cause of UGIB and highlights the multidisciplinary management of gastrointestinal bleeding in the setting of a negative endoscopic evaluation. VCE is increasingly utilized to investigate small bowel bleeds; however, one must be cautious with this approach, particularly in patients predisposed to adhesions or strictures due to history of major abdominal surgeries or chronic inflammatory states (i.e., Crohn’s). Recognizing factors contributing to pseudoaneurysm formation (i.e., trauma, infection, procedures with vascular manipulation), and therefore potential fistula development, is critical for guiding timely appropriate imaging and surgical involvement, as demonstrated in this case with focused imaging that prompted an operative intervention.
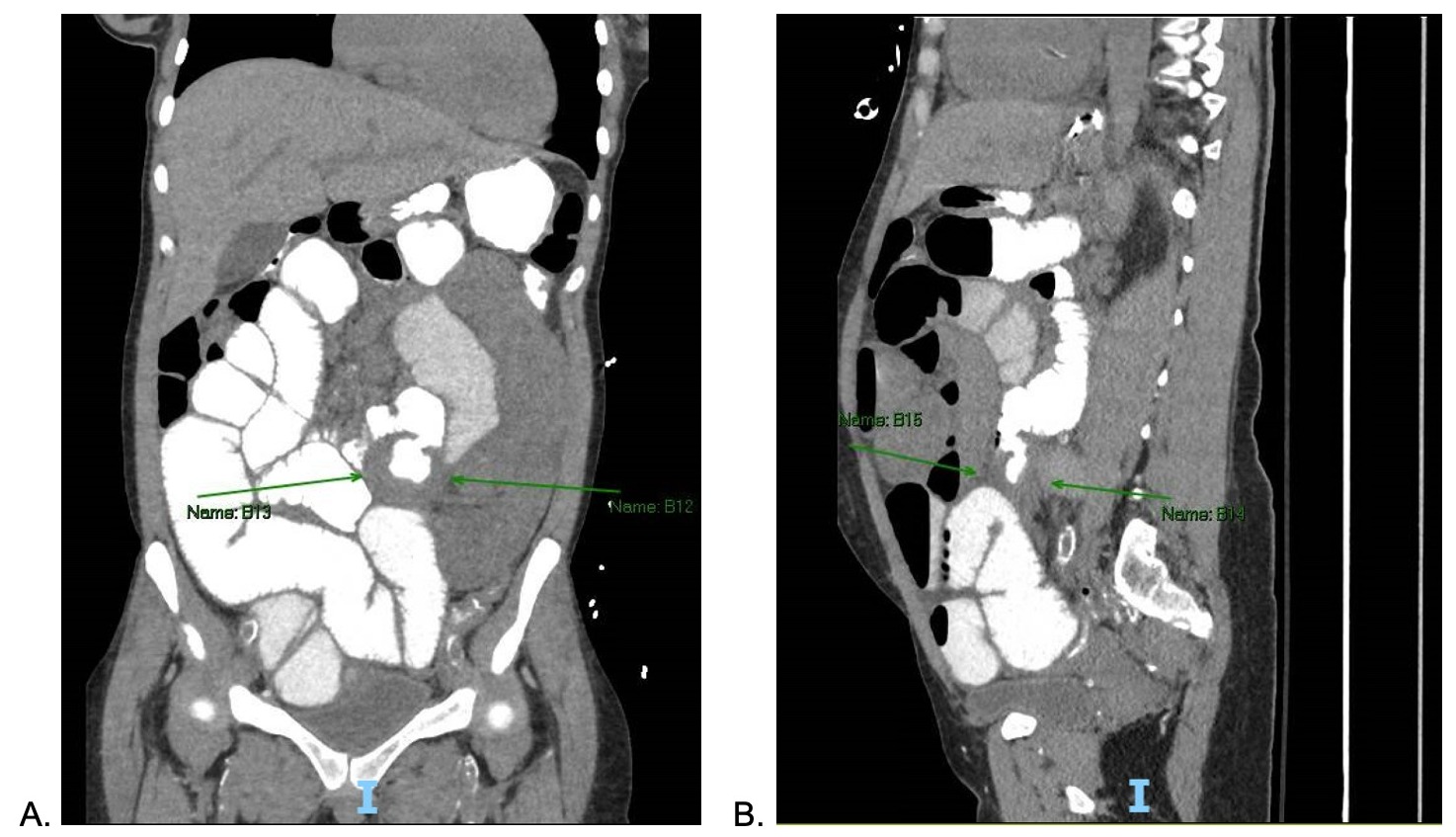
Figure: Figure 1. CT Abdomen Pelvis with PO Contrast in coronal (A) and sagittal (B) views demonstrating persistent small bowel obstruction and extravasation of enteric contrast into the pseudoaneurysm.
Disclosures:
Rhea Fogla indicated no relevant financial relationships.
Eliza Cricco-Lizza indicated no relevant financial relationships.
Carl Crawford: Ferring – Grant/Research Support. Nestle – Speakers Bureau. Phathom – Speakers Bureau. Seres – Speakers Bureau. Vedanta – Grant/Research Support.
Rhea Fogla, MD, Eliza Cricco-Lizza, MD, Carl V. Crawford, MD. P4249 - Fistula Formation Between Small Bowel and Pseudoaneurysm as a Source of an Upper Gastrointestinal Bleed, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
