Tuesday Poster Session
Category: GI Bleeding
P4250 - A Non-Ampullary Duodenal Polyp as a Source of Bleeding in Alcohol-Associated Cirrhosis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Rhea Fogla, MD
New York-Presbyterian / Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Rhea Fogla, MD1, Emily Smith, MD2, Emily Schonfeld, MD1, Arun B.. Jesudian, MD3, SriHari Mahadev, MD1, Cynthia O. Akagbosu, MD, MA1, David Wan, MD1
1New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian/Weill Cornell, New York, NY; 3Weill Cornell Medicine, New York, NY
Introduction: Upper gastrointestinal bleeding (UGIB) is a common cause of morbidity and mortality in patients with cirrhosis and variceal hemorrhage has been shown to have a high mortality rate. While variceal hemorrhage is commonly encountered, consideration of nonvariceal sources of UGIB is imperative. Here, we present a case of a non-ampullary duodenal polyp as a source of UGIB in a patient with decompensated cirrhosis.
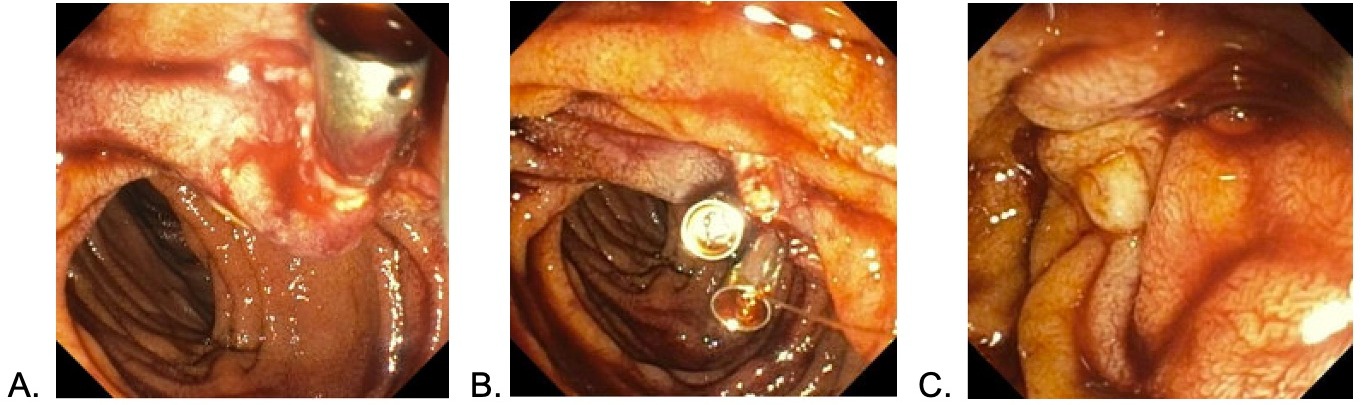
Case Description/Methods: A 47-year-old male with a past medical history of alcohol-associated cirrhosis complicated by ascites and an esophageal variceal bleed status post band ligation two days prior to presentation, umbilical hernia, and chronic kidney disease, presented with abdominal pain and melena. Labs were notable for hemoglobin of 6.5 g/mL, platelets 69,000/μL, BUN 92 mg/dL, creatinine 3.35 mg/dL, sodium 136 mmol/L, total bilirubin 0.9 mg/dL, and INR 2.3. On exam, the patient was found to have an incarcerated umbilical hernia, requiring emergent exploratory laparotomy and repair. His course was complicated by persistent melena, for which he was empirically treated with pantoprazole, ceftriaxone, and octreotide. His initial upper endoscopy (EGD) excluded esophageal variceal or post-banding ulcer bleeding as sources of the UGIB. A repeat EGD to address ongoing hemorrhage revealed two bleeding sessile polyps believed to originate from the papilla. Further examination with a side-viewing duodenoscope demonstrated that the polyps were adjacent to the ampulla of Vater. These polyps were resected, and hemostasis was achieved with epinephrine injection and placement of two hemostatic clips. Recurrent bleeding prompted a repeat EGD the following day, which identified oozing at the site of the polypectomy and was subsequently treated with bipolar cautery. The patient’s course was complicated by the development of hepatorenal syndrome-acute kidney injury, and he ultimately underwent a simultaneous liver-kidney transplant.
Discussion: Maintaining a broad differential diagnosis including nonvariceal causes of UGIB in cirrhosis is essential. Duodenal polyps are often asymptomatic and found incidentally, but can present with bleeding. Proper visualization and identification of the lesion often requires utilization of a side-viewing duodenoscope. Although a rare cause of UGIB in cirrhosis, proper investigation for sources of nonvariceal bleeding can identify and address duodenal polyp-associated bleeding in this population.
Disclosures:
Rhea Fogla, MD1, Emily Smith, MD2, Emily Schonfeld, MD1, Arun B.. Jesudian, MD3, SriHari Mahadev, MD1, Cynthia O. Akagbosu, MD, MA1, David Wan, MD1. P4250 - A Non-Ampullary Duodenal Polyp as a Source of Bleeding in Alcohol-Associated Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian/Weill Cornell, New York, NY; 3Weill Cornell Medicine, New York, NY
Introduction: Upper gastrointestinal bleeding (UGIB) is a common cause of morbidity and mortality in patients with cirrhosis and variceal hemorrhage has been shown to have a high mortality rate. While variceal hemorrhage is commonly encountered, consideration of nonvariceal sources of UGIB is imperative. Here, we present a case of a non-ampullary duodenal polyp as a source of UGIB in a patient with decompensated cirrhosis.
Case Description/Methods: A 47-year-old male with a past medical history of alcohol-associated cirrhosis complicated by ascites and an esophageal variceal bleed status post band ligation two days prior to presentation, umbilical hernia, and chronic kidney disease, presented with abdominal pain and melena. Labs were notable for hemoglobin of 6.5 g/mL, platelets 69,000/μL, BUN 92 mg/dL, creatinine 3.35 mg/dL, sodium 136 mmol/L, total bilirubin 0.9 mg/dL, and INR 2.3. On exam, the patient was found to have an incarcerated umbilical hernia, requiring emergent exploratory laparotomy and repair. His course was complicated by persistent melena, for which he was empirically treated with pantoprazole, ceftriaxone, and octreotide. His initial upper endoscopy (EGD) excluded esophageal variceal or post-banding ulcer bleeding as sources of the UGIB. A repeat EGD to address ongoing hemorrhage revealed two bleeding sessile polyps believed to originate from the papilla. Further examination with a side-viewing duodenoscope demonstrated that the polyps were adjacent to the ampulla of Vater. These polyps were resected, and hemostasis was achieved with epinephrine injection and placement of two hemostatic clips. Recurrent bleeding prompted a repeat EGD the following day, which identified oozing at the site of the polypectomy and was subsequently treated with bipolar cautery. The patient’s course was complicated by the development of hepatorenal syndrome-acute kidney injury, and he ultimately underwent a simultaneous liver-kidney transplant.
Discussion: Maintaining a broad differential diagnosis including nonvariceal causes of UGIB in cirrhosis is essential. Duodenal polyps are often asymptomatic and found incidentally, but can present with bleeding. Proper visualization and identification of the lesion often requires utilization of a side-viewing duodenoscope. Although a rare cause of UGIB in cirrhosis, proper investigation for sources of nonvariceal bleeding can identify and address duodenal polyp-associated bleeding in this population.
Figure: Figure 1. Upper endoscopy revealing sessile polyps at the area of the papilla with evidence of bleeding.
Disclosures:
Rhea Fogla indicated no relevant financial relationships.
Emily Smith indicated no relevant financial relationships.
Emily Schonfeld indicated no relevant financial relationships.
Arun Jesudian: Bausch Health – Consultant. Madrigal Pharmaceuticals – Speakers Bureau. Novo Nordisk – Advisor or Review Panel Member, Consultant. Orphalan – Advisor or Review Panel Member, Consultant. Salix Pharmaceuticals – Consultant, Speakers Bureau.
SriHari Mahadev: Boston Scientific – Consultant. Conmed – Consultant.
Cynthia Akagbosu indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Rhea Fogla, MD1, Emily Smith, MD2, Emily Schonfeld, MD1, Arun B.. Jesudian, MD3, SriHari Mahadev, MD1, Cynthia O. Akagbosu, MD, MA1, David Wan, MD1. P4250 - A Non-Ampullary Duodenal Polyp as a Source of Bleeding in Alcohol-Associated Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
