Tuesday Poster Session
Category: GI Bleeding
P4252 - ANCA-Associated Vasculitis Flare Presenting as Refractory Gastrointestinal Bleeding
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- CB
Charizza Grace Besmanos, MD
University of California San Francisco
Fresno, CA
Presenting Author(s)
Charizza Grace Besmanos, MD1, Srikar Sama, MD1, Candice Reyes, MD2
1University of California San Francisco, Fresno, CA; 2University of California San Francisco and San Francisco VA Health Care System, Fresno, CA
Introduction: ANCA-associated vasculitis (AAV), a type of necrotizing vasculitis primarily affects small blood vessels. AAV is associated with antineutrophilic cytoplasmic antibody (ANCA) that is specific for myeloperoxidase (MPO) or proteinase 3 (PR3). AAV may present with systemic inflammatory symptoms or specific features of multiple end-organ damage. Gastrointestinal (GI) involvement is seen in 5-10% of patients with granulomatosis with polyangiitis (GPA), and AAV flare presenting as an upper GI bleed is uncommon.
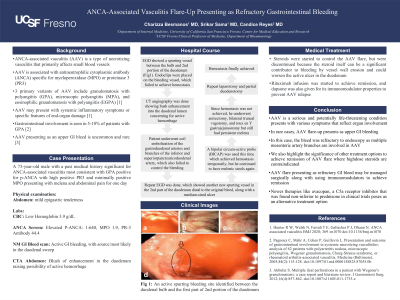
Case Description/Methods: 73-year-old male with AAV most consistent with GPA (positive for p-ANCA with high positive PR3 and minimally positive MPO) presented to the hospital with one day of melena and abdominal pain. Initial workup revealed hemoglobin of 3.9 g/dL. Esophagogastroduodenoscopy (EGD) showed a spurting vessel between the bulb and second portion of the duodenum. Endoclips were placed which failed to stop the bleeding. Computed tomography (CT) angiography showed blush enhancement extending into the duodenal lumen concerning for active hemorrhage. He underwent coil embolization of the gastroduodenal arteries and branches of the superior and inferior pancreaticoduodenal artery, however bleeding continued. A repeat EGD revealed new spurting vessel in the second part of the duodenum distal to the original bleed, along with a medium-sized ulcer. A bipolar circum-active probe (BICAP) was done without success, followed by epinephrine, hemospray and endoclips placement achieving temporary hemostasis, but he continued to have melena. As hemostasis was not achieved, he underwent antrectomy, bilateral truncal vagotomy and roux-en-Y gastrojejunostomy but still had persistent melena. Finally, hemostasis was achieved with repeat laparotomy and partial duodenectomy. Rituximab infusion was started to achieve remission; dapsone was also given for its immunomodulator properties to prevent AAV relapse.
Discussion: In rare cases, AAV flares may present as upper GI bleeding. In this case, the bleed was refractory as different mesenteric artery branches are involved. We also highlight the significance of other treatment options such as rituximab to achieve remission of AAV flare where high-dose steroids are contraindicated. AAV flare presenting as refractory GI bleed may be managed surgically along with using immunomodulators to achieve remission. Newer therapies like avacopan, a C5a receptor inhibitor that was found non-inferior to prednisone in clinical trials poses as an alternative treatment option.
Disclosures:
Charizza Grace Besmanos, MD1, Srikar Sama, MD1, Candice Reyes, MD2. P4252 - ANCA-Associated Vasculitis Flare Presenting as Refractory Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of California San Francisco, Fresno, CA; 2University of California San Francisco and San Francisco VA Health Care System, Fresno, CA
Introduction: ANCA-associated vasculitis (AAV), a type of necrotizing vasculitis primarily affects small blood vessels. AAV is associated with antineutrophilic cytoplasmic antibody (ANCA) that is specific for myeloperoxidase (MPO) or proteinase 3 (PR3). AAV may present with systemic inflammatory symptoms or specific features of multiple end-organ damage. Gastrointestinal (GI) involvement is seen in 5-10% of patients with granulomatosis with polyangiitis (GPA), and AAV flare presenting as an upper GI bleed is uncommon.
Case Description/Methods: 73-year-old male with AAV most consistent with GPA (positive for p-ANCA with high positive PR3 and minimally positive MPO) presented to the hospital with one day of melena and abdominal pain. Initial workup revealed hemoglobin of 3.9 g/dL. Esophagogastroduodenoscopy (EGD) showed a spurting vessel between the bulb and second portion of the duodenum. Endoclips were placed which failed to stop the bleeding. Computed tomography (CT) angiography showed blush enhancement extending into the duodenal lumen concerning for active hemorrhage. He underwent coil embolization of the gastroduodenal arteries and branches of the superior and inferior pancreaticoduodenal artery, however bleeding continued. A repeat EGD revealed new spurting vessel in the second part of the duodenum distal to the original bleed, along with a medium-sized ulcer. A bipolar circum-active probe (BICAP) was done without success, followed by epinephrine, hemospray and endoclips placement achieving temporary hemostasis, but he continued to have melena. As hemostasis was not achieved, he underwent antrectomy, bilateral truncal vagotomy and roux-en-Y gastrojejunostomy but still had persistent melena. Finally, hemostasis was achieved with repeat laparotomy and partial duodenectomy. Rituximab infusion was started to achieve remission; dapsone was also given for its immunomodulator properties to prevent AAV relapse.
Discussion: In rare cases, AAV flares may present as upper GI bleeding. In this case, the bleed was refractory as different mesenteric artery branches are involved. We also highlight the significance of other treatment options such as rituximab to achieve remission of AAV flare where high-dose steroids are contraindicated. AAV flare presenting as refractory GI bleed may be managed surgically along with using immunomodulators to achieve remission. Newer therapies like avacopan, a C5a receptor inhibitor that was found non-inferior to prednisone in clinical trials poses as an alternative treatment option.
Disclosures:
Charizza Grace Besmanos indicated no relevant financial relationships.
Srikar Sama indicated no relevant financial relationships.
Candice Reyes indicated no relevant financial relationships.
Charizza Grace Besmanos, MD1, Srikar Sama, MD1, Candice Reyes, MD2. P4252 - ANCA-Associated Vasculitis Flare Presenting as Refractory Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
