Tuesday Poster Session
Category: GI Bleeding
P4254 - A Gastrointestinal Bleeding Mystery: Uncovering Localized Gastric Amyloidosis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Nader Mekheal, MD
St. Joseph's University Medical Center
Paterson, NJ
Presenting Author(s)
Nader Mekheal, MD1, Lefika Bathobakae, MD1, Alisa Farokhian, MD2, Mina Alkomos, MD2, Mohamed Elagami, MD1, Ariy Volfson, MD1, Walid Baddoura, MD2, Yana Cavanagh, MD2
1St. Joseph's University Medical Center, Paterson, NJ; 2St. Joseph's University Medical Center, Paterson, NJ
Introduction: Amyloidosis is caused by abnormal extracellular protein deposition. While gastrointestinal involvement is common in systemic disease, localized gastric amyloidosis (LGA) is very rare. Diagnosing and managing LGA can be challenging. Here, we present a case of LGA presenting with upper gastrointestinal bleeding.
Case Description/Methods: A 79-year-old female with a medical history of dyslipidemia, hypertension, morbid obesity, and depression presented to the ED following an episode of coffee-ground emesis and dark stools. In the ED, she was tachycardic but hemodynamically stable. Laboratory tests revealed a hemoglobin level of 7.6 g/dL, which improved to 9.6 g/dL after receiving 2 units of packed red blood cells. A CT angiogram of the abdomen indicated questionable contrast pooling in the jejunum.
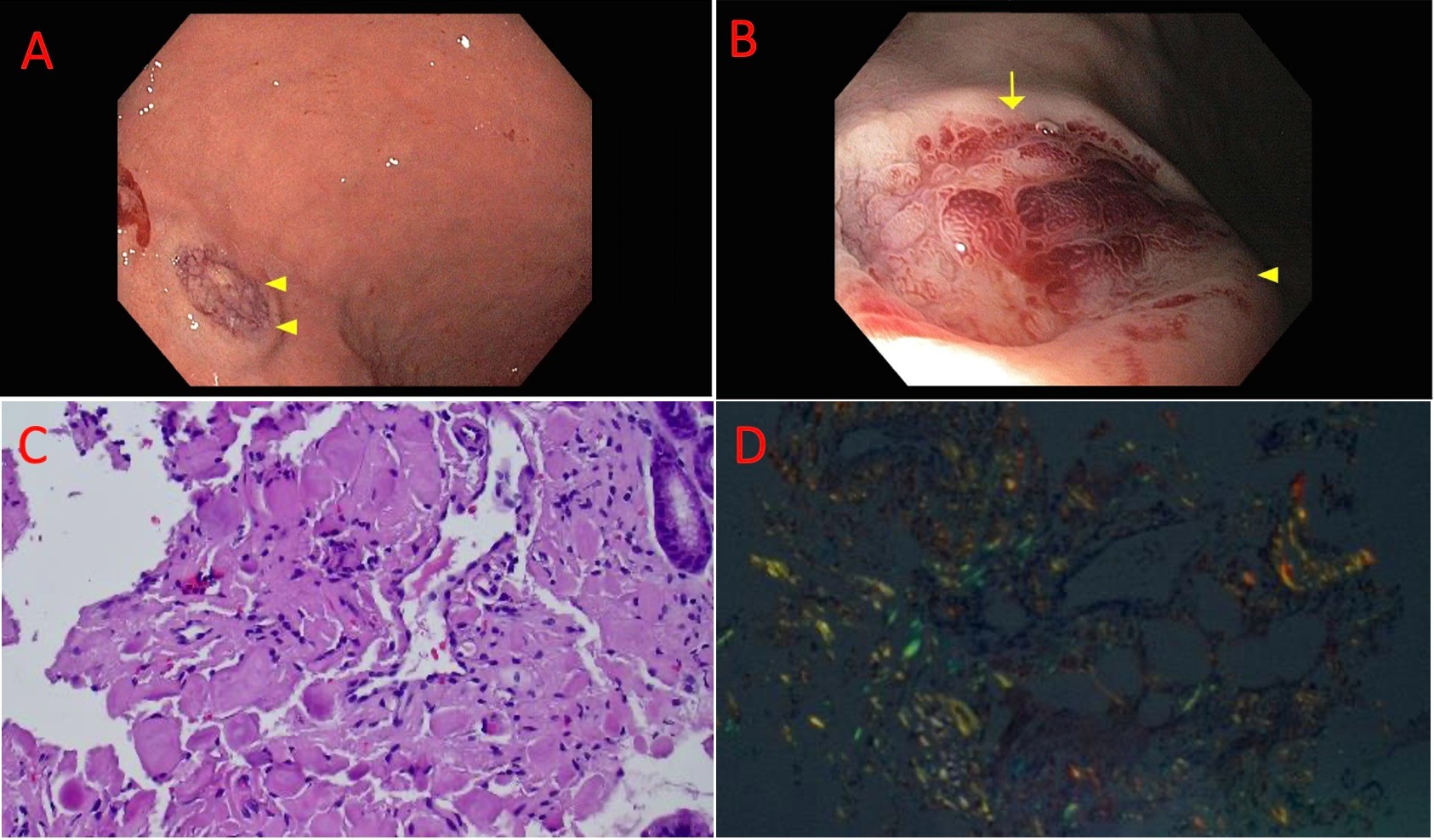
The patient was evaluated by gastroenterology, and an esophagogastroduodenoscopy (EGD) showed bluish discoloration of the gastric mucosa in the gastric fundus and greater curvature, along with crated lesions, one of which was actively oozing blood. This lesion was treated with epinephrine injection and argon plasma coagulation (APC) (Figure 1). A biopsy confirmed the presence of amyloid deposits (Figure 1). Follow-up tests, including a renal ultrasound, echocardiography and radiography, were negative, and urine tests showed no proteinuria. The patient was discharged on pantoprazole and close follow-up to further management.
Discussion: Amyloidosis is a group of diseases caused by protein folding disorders, leading to the buildup of insoluble fibrils in tissues and organs. These deposits can disrupt normal tissue structure, and cause organ dysfunction. While gastrointestinal involvement is common in systemic amyloidosis, it is rare in localized cases. Localized gastric amyloidosis (LGA) is particularly uncommon.
LGA's clinical signs are non-specific and can resemble other gastric diseases. Symptoms can vary from none at all to epigastric discomfort, pain, weight loss, anemia, heartburn, nausea, hematemesis, dark stools, and fatigue. Diagnosing LGA is difficult and usually starts with incidental detection during an endoscopy, followed by tests to exclude systemic involvement. In our patient, initial tests are suggestive for LGA, and further imaging were negative for systemic involvement.
Treatment for amyloidosis aims to remove harmful amyloid deposits and restore normal organ function as much as possible. Options include surgery, observation, and radiotherapy.
Disclosures:
Nader Mekheal, MD1, Lefika Bathobakae, MD1, Alisa Farokhian, MD2, Mina Alkomos, MD2, Mohamed Elagami, MD1, Ariy Volfson, MD1, Walid Baddoura, MD2, Yana Cavanagh, MD2. P4254 - A Gastrointestinal Bleeding Mystery: Uncovering Localized Gastric Amyloidosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Joseph's University Medical Center, Paterson, NJ; 2St. Joseph's University Medical Center, Paterson, NJ
Introduction: Amyloidosis is caused by abnormal extracellular protein deposition. While gastrointestinal involvement is common in systemic disease, localized gastric amyloidosis (LGA) is very rare. Diagnosing and managing LGA can be challenging. Here, we present a case of LGA presenting with upper gastrointestinal bleeding.
Case Description/Methods: A 79-year-old female with a medical history of dyslipidemia, hypertension, morbid obesity, and depression presented to the ED following an episode of coffee-ground emesis and dark stools. In the ED, she was tachycardic but hemodynamically stable. Laboratory tests revealed a hemoglobin level of 7.6 g/dL, which improved to 9.6 g/dL after receiving 2 units of packed red blood cells. A CT angiogram of the abdomen indicated questionable contrast pooling in the jejunum.
The patient was evaluated by gastroenterology, and an esophagogastroduodenoscopy (EGD) showed bluish discoloration of the gastric mucosa in the gastric fundus and greater curvature, along with crated lesions, one of which was actively oozing blood. This lesion was treated with epinephrine injection and argon plasma coagulation (APC) (Figure 1). A biopsy confirmed the presence of amyloid deposits (Figure 1). Follow-up tests, including a renal ultrasound, echocardiography and radiography, were negative, and urine tests showed no proteinuria. The patient was discharged on pantoprazole and close follow-up to further management.
Discussion: Amyloidosis is a group of diseases caused by protein folding disorders, leading to the buildup of insoluble fibrils in tissues and organs. These deposits can disrupt normal tissue structure, and cause organ dysfunction. While gastrointestinal involvement is common in systemic amyloidosis, it is rare in localized cases. Localized gastric amyloidosis (LGA) is particularly uncommon.
LGA's clinical signs are non-specific and can resemble other gastric diseases. Symptoms can vary from none at all to epigastric discomfort, pain, weight loss, anemia, heartburn, nausea, hematemesis, dark stools, and fatigue. Diagnosing LGA is difficult and usually starts with incidental detection during an endoscopy, followed by tests to exclude systemic involvement. In our patient, initial tests are suggestive for LGA, and further imaging were negative for systemic involvement.
Treatment for amyloidosis aims to remove harmful amyloid deposits and restore normal organ function as much as possible. Options include surgery, observation, and radiotherapy.
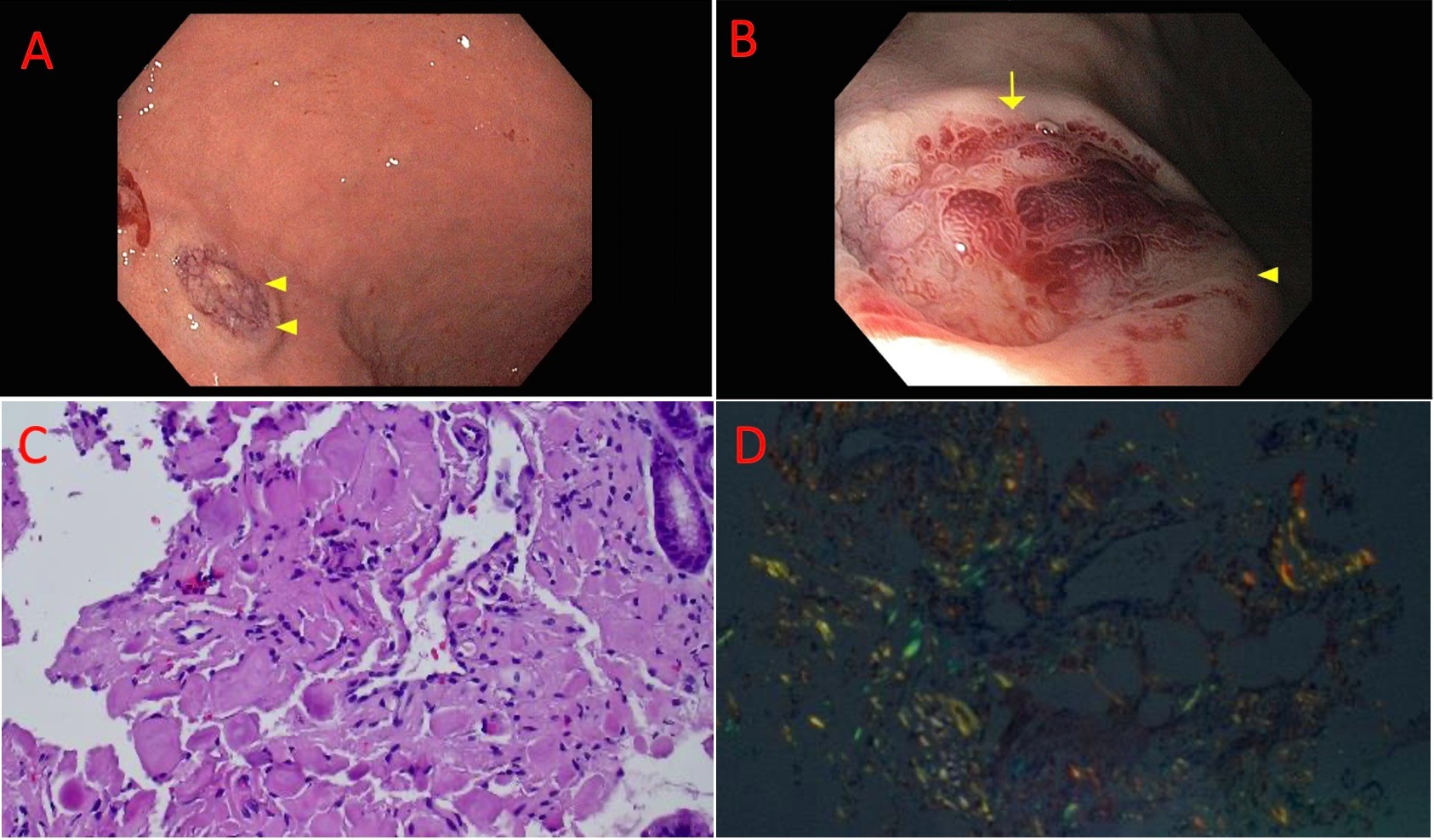
Figure: Figure 1: A: Crated gastric lesion with bluish discoloration; B: evidence of bleeding from abnormal gastric mucosa; C: H&E staining demonstrating deposition of amyloid fibrous connective tissue in the interstitium with inflammatory cell infiltration; D: Congo red staining positive for amyloid protein
Disclosures:
Nader Mekheal indicated no relevant financial relationships.
Lefika Bathobakae indicated no relevant financial relationships.
Alisa Farokhian indicated no relevant financial relationships.
Mina Alkomos indicated no relevant financial relationships.
Mohamed Elagami indicated no relevant financial relationships.
Ariy Volfson indicated no relevant financial relationships.
Walid Baddoura indicated no relevant financial relationships.
Yana Cavanagh indicated no relevant financial relationships.
Nader Mekheal, MD1, Lefika Bathobakae, MD1, Alisa Farokhian, MD2, Mina Alkomos, MD2, Mohamed Elagami, MD1, Ariy Volfson, MD1, Walid Baddoura, MD2, Yana Cavanagh, MD2. P4254 - A Gastrointestinal Bleeding Mystery: Uncovering Localized Gastric Amyloidosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

