Tuesday Poster Session
Category: IBD
P4257 - Disease Characterization and Safety Contextualization in Patients with Ulcerative Colitis Using a Healthcare Administrative Database in the United States
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Miguel Regueiro, MD
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Miguel D Regueiro, MD1, Meenakshi Bewtra, MD2, Marla C. Dubinsky, MD3, Xiang Guo, PharmD, MS4, Chunyang Feng, 5, Aoibhinn McDonnell, PhD6, Milena Gianfrancesco, PhD, MPH5
1Cleveland Clinic, Cleveland, OH; 2University of Pennsylvania, Philadelphia, PA; 3Icahn School of Medicine at Mount Sinai, New York, NY; 4Pfizer Inc., Collegeville, PA; 5Pfizer Inc., New York, NY; 6Pfizer Ltd., Sandwich, England, United Kingdom
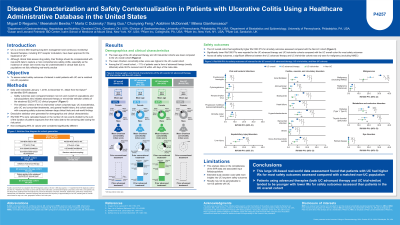
Introduction: Several therapies have been recently approved for ulcerative colitis (UC).1 Although clinical trials assess drug safety, they should be contextualized with real‑world data (RWD), especially as many rare events are not commonly reported in clinical trials.
Methods: This retrospective, observational study aimed to use RWD to investigate safety outcomes in four cohorts; three for patients with UC: (1) those receiving any treatment (UC overall), (2) those receiving advanced therapies (UC advanced therapy), and (3) those meeting the selection criteria of the etrasimod ELEVATE UC clinical program2 (UC trial similar); the fourth cohort comprised individuals without UC (non-UC; Table). Data were extracted (1/1/2016–12/31/2022) from the United States Optum electronic health record database. Demographic data were summarized descriptively. Incidence rates per 1000 patient‑years were calculated (Table).
Results: Data from 32,170 (UC overall), 3,332 (UC advanced therapy), 1,435 (UC trial similar), and 160,795 (non-UC) individuals were included. Cohorts were well balanced regarding sex (female: 48.5% – 54.5%) and were mostly White (86.3% – 86.8%) with mean ages of 52.3 (UC overall), 45.0 (UC advanced therapy), 44.0 (UC trial similar), and 52.3 (non-UC) years. The UC overall cohort had numerically the highest rates across nearly all selected safety outcomes (Table). The non-UC and UC trial similar cohorts had generally comparable rates followed by the UC advanced therapy cohort for cardiac, vascular, and circulatory disorders and metabolism and endocrine disorders. These three cohorts had similar rates for rare outcomes: cryptococcal meningitis, progressive multifocal leukoencephalopathy, malignancy (cutaneous), and retinal diseases (Table). Generally, all UC cohorts had numerically higher rates vs the non-UC cohort for most infections and liver injuries (Table).
Discussion: This large-population RWD assessment comprising common and rarely observed safety events found that patients with UC had higher rates for most outcomes vs a matched non-UC population. Overall, the UC advanced therapy and UC trial similar cohorts had lower rates of safety events vs the UC overall cohort and were more comparable to the non-UC cohort. These findings assist in understanding the background risks of safety events in patients with UC, allowing contextualization with clinical trial data and future RWD.
References:
1. Ferretti F et al. J Clin Med 2022; 11: 2302.
2. Sandborn WJ et al. Lancet 2023; 401: 1159–1171.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Miguel D Regueiro, MD1, Meenakshi Bewtra, MD2, Marla C. Dubinsky, MD3, Xiang Guo, PharmD, MS4, Chunyang Feng, 5, Aoibhinn McDonnell, PhD6, Milena Gianfrancesco, PhD, MPH5. P4257 - Disease Characterization and Safety Contextualization in Patients with Ulcerative Colitis Using a Healthcare Administrative Database in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2University of Pennsylvania, Philadelphia, PA; 3Icahn School of Medicine at Mount Sinai, New York, NY; 4Pfizer Inc., Collegeville, PA; 5Pfizer Inc., New York, NY; 6Pfizer Ltd., Sandwich, England, United Kingdom
Introduction: Several therapies have been recently approved for ulcerative colitis (UC).1 Although clinical trials assess drug safety, they should be contextualized with real‑world data (RWD), especially as many rare events are not commonly reported in clinical trials.
Methods: This retrospective, observational study aimed to use RWD to investigate safety outcomes in four cohorts; three for patients with UC: (1) those receiving any treatment (UC overall), (2) those receiving advanced therapies (UC advanced therapy), and (3) those meeting the selection criteria of the etrasimod ELEVATE UC clinical program2 (UC trial similar); the fourth cohort comprised individuals without UC (non-UC; Table). Data were extracted (1/1/2016–12/31/2022) from the United States Optum electronic health record database. Demographic data were summarized descriptively. Incidence rates per 1000 patient‑years were calculated (Table).
Results: Data from 32,170 (UC overall), 3,332 (UC advanced therapy), 1,435 (UC trial similar), and 160,795 (non-UC) individuals were included. Cohorts were well balanced regarding sex (female: 48.5% – 54.5%) and were mostly White (86.3% – 86.8%) with mean ages of 52.3 (UC overall), 45.0 (UC advanced therapy), 44.0 (UC trial similar), and 52.3 (non-UC) years. The UC overall cohort had numerically the highest rates across nearly all selected safety outcomes (Table). The non-UC and UC trial similar cohorts had generally comparable rates followed by the UC advanced therapy cohort for cardiac, vascular, and circulatory disorders and metabolism and endocrine disorders. These three cohorts had similar rates for rare outcomes: cryptococcal meningitis, progressive multifocal leukoencephalopathy, malignancy (cutaneous), and retinal diseases (Table). Generally, all UC cohorts had numerically higher rates vs the non-UC cohort for most infections and liver injuries (Table).
Discussion: This large-population RWD assessment comprising common and rarely observed safety events found that patients with UC had higher rates for most outcomes vs a matched non-UC population. Overall, the UC advanced therapy and UC trial similar cohorts had lower rates of safety events vs the UC overall cohort and were more comparable to the non-UC cohort. These findings assist in understanding the background risks of safety events in patients with UC, allowing contextualization with clinical trial data and future RWD.
References:
1. Ferretti F et al. J Clin Med 2022; 11: 2302.
2. Sandborn WJ et al. Lancet 2023; 401: 1159–1171.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Miguel D Regueiro: AbbVie – Advisory Committee/Board Member, Consultant, Speakers Bureau.
Meenakshi Bewtra: AbbVie – Consultant, Honorarium – CME Program. Bristol Myers Squibb – Consultant. CME program (sponsored by AbbVie) – Honorarium – CME Program. GlaxoSmith Kline – Grant/Research Support. Iterative Scopes – Grant/Research Support. Janssen – Grant/Research Support. Johnson & Johnson – Consultant. MedEd – Consultant. Pfizer Inc – Consultant. Takeda – Grant/Research Support.
Marla Dubinsky: AbbVie – Consultant. Abivax – Consultant. Arena – Consultant. AstraZeneca – Consultant. Bristol Myers Squibb – Consultant. Celgene – Consultant. Eli Lilly – Consultant. Genentech – Consultant. Gilead – Consultant. Janssen – Consultant. Pfizer Inc – Consultant. Prometheus Labs – Consultant. Takeda – Consultant.
Xiang Guo: Pfizer Inc – Employee, Stock Options.
Chunyang Feng: Pfizer Inc – Employee, Stock Options.
Aoibhinn McDonnell: Pfizer Inc – Stock Options. Pfizer Ltd – Employee.
Milena Gianfrancesco: Pfizer Inc – Employee, Stock Options.
Miguel D Regueiro, MD1, Meenakshi Bewtra, MD2, Marla C. Dubinsky, MD3, Xiang Guo, PharmD, MS4, Chunyang Feng, 5, Aoibhinn McDonnell, PhD6, Milena Gianfrancesco, PhD, MPH5. P4257 - Disease Characterization and Safety Contextualization in Patients with Ulcerative Colitis Using a Healthcare Administrative Database in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
