Tuesday Poster Session
Category: IBD
P4260 - Compliance Rate of Venous Thromboembolism Prevention in Hospitalized Patients With Inflammatory Bowel Disease in a Community Hospital Setting
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Aria Jalalian, MD
Lankenau Medical Center
Wynnewood, PA
Presenting Author(s)
Aria Jalalian, MD, Julian Remouns, DO, Patricia Wong, MD, MSc(Epi)
Lankenau Medical Center, Wynnewood, PA
Introduction: Patients with inflammatory bowel disease (IBD) are at a 2 to 8.4-fold increased risk for venous thromboembolism (VTE) compared to the general population. VTE in hospitalized IBD patients is associated with increased morbidity, mortality, and extended hospital stays. For these reasons, multiple medical societies recommend chemical VTE prophylaxis in all hospitalized IBD patients. Despite this, many patients do not receive chemical VTE prophylaxis, possibly due to a lack of physician awareness or concerns about increasing the risk of gastrointestinal bleeding.
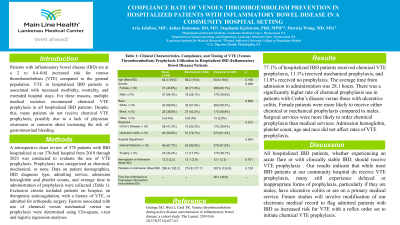
Methods: A retrospective chart review of 578 patients with IBD hospitalized at our 370-bed hospital from 2019 through 2023 was conducted to evaluate the use of VTE prophylaxis. Prophylaxis was categorized as chemical, mechanical, or none. Data on patient demographics, IBD diagnosis type, admitting service, admission hemoglobin and platelet counts, and average time to administration of prophylaxis were collected (Table 1). Exclusion criteria included patients on hospice, on therapeutic anticoagulation, with a history of VTE, or admitted for orthopedic surgery. Factors associated with use of chemical versus mechanical versus no prophylaxis were determined using Chi-square, t-test and logistic regression analyses.
Results: Approximately 78% of hospitalized IBD patients received chemical VTE prophylaxis, 11.1% received mechanical prophylaxis, and 11.8% received no prophylaxis. The average time from admission to administration was 28.1 hours. There was a significantly higher rate of chemical prophylaxis use in Crohn’s disease patients versus ulcerative colitis. Female patients were more likely to receive either chemical or mechanical prophylaxis compared to males. There was no significant difference in chemical prophylaxis rate between medical and surgical services. Admission hemoglobin, platelet count, age and race did not affect rates of VTE prophylaxis.
Discussion: All hospitalized IBD patients, whether experiencing an acute flare or with clinically stable IBD, should receive VTE prophylaxis . Our results indicate that while most IBD patients at our community hospital do receive VTE prophylaxis, many still experience delayed or inappropriate forms of prophylaxis. Future studies will involve modification of our electronic medical record to flag admitted patients with IBD as increased risk for VTE with a reflex order set to initiate chemical VTE prophylaxis.
Grainge, M. et al. VTE during active disease and remission in IBD, 2010, 657-663.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Aria Jalalian, MD, Julian Remouns, DO, Patricia Wong, MD, MSc(Epi). P4260 - Compliance Rate of Venous Thromboembolism Prevention in Hospitalized Patients With Inflammatory Bowel Disease in a Community Hospital Setting, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Lankenau Medical Center, Wynnewood, PA
Introduction: Patients with inflammatory bowel disease (IBD) are at a 2 to 8.4-fold increased risk for venous thromboembolism (VTE) compared to the general population. VTE in hospitalized IBD patients is associated with increased morbidity, mortality, and extended hospital stays. For these reasons, multiple medical societies recommend chemical VTE prophylaxis in all hospitalized IBD patients. Despite this, many patients do not receive chemical VTE prophylaxis, possibly due to a lack of physician awareness or concerns about increasing the risk of gastrointestinal bleeding.
Methods: A retrospective chart review of 578 patients with IBD hospitalized at our 370-bed hospital from 2019 through 2023 was conducted to evaluate the use of VTE prophylaxis. Prophylaxis was categorized as chemical, mechanical, or none. Data on patient demographics, IBD diagnosis type, admitting service, admission hemoglobin and platelet counts, and average time to administration of prophylaxis were collected (Table 1). Exclusion criteria included patients on hospice, on therapeutic anticoagulation, with a history of VTE, or admitted for orthopedic surgery. Factors associated with use of chemical versus mechanical versus no prophylaxis were determined using Chi-square, t-test and logistic regression analyses.
Results: Approximately 78% of hospitalized IBD patients received chemical VTE prophylaxis, 11.1% received mechanical prophylaxis, and 11.8% received no prophylaxis. The average time from admission to administration was 28.1 hours. There was a significantly higher rate of chemical prophylaxis use in Crohn’s disease patients versus ulcerative colitis. Female patients were more likely to receive either chemical or mechanical prophylaxis compared to males. There was no significant difference in chemical prophylaxis rate between medical and surgical services. Admission hemoglobin, platelet count, age and race did not affect rates of VTE prophylaxis.
Discussion: All hospitalized IBD patients, whether experiencing an acute flare or with clinically stable IBD, should receive VTE prophylaxis . Our results indicate that while most IBD patients at our community hospital do receive VTE prophylaxis, many still experience delayed or inappropriate forms of prophylaxis. Future studies will involve modification of our electronic medical record to flag admitted patients with IBD as increased risk for VTE with a reflex order set to initiate chemical VTE prophylaxis.
Grainge, M. et al. VTE during active disease and remission in IBD, 2010, 657-663.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Aria Jalalian indicated no relevant financial relationships.
Julian Remouns indicated no relevant financial relationships.
Patricia Wong indicated no relevant financial relationships.
Aria Jalalian, MD, Julian Remouns, DO, Patricia Wong, MD, MSc(Epi). P4260 - Compliance Rate of Venous Thromboembolism Prevention in Hospitalized Patients With Inflammatory Bowel Disease in a Community Hospital Setting, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

