Monday Poster Session
Category: Interventional Endoscopy
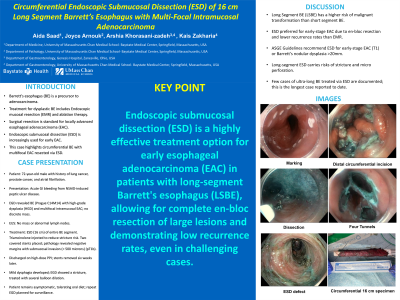
P2851 - Circumferential Endoscopic Submucosal Dissection (ESD) of 15-cm Long Segment Barrett’s Esophagus With Multi-Focal Intramucosal Adenocarcinoma
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Aida Saad, MD
Baystate Medical Center
Enfield, CT
Presenting Author(s)
Award: Presidential Poster Award
Aida Saad, MD1, Arshia Khorasanizadeh, MD2, Kais Zakharia, MD3, Joyce Arnouk, 4
1Baystate Medical Center, Enfield, CT; 2UMass Chan, Baystate, Springfield, MA; 3Baystate Medical Center, Springfield, MA; 4Westfield, MA
Introduction: Barret's esophagus (BE) is a well-known precursor of adenocarcinoma. Endoscopic mucosal resection (EMR) and ablation therapy (radiofrequency ablation and cryotherapy) are the mainstay of treatment for dysplastic BE. For patients with locally advanced esophageal adenocarcinoma (EAC), surgical resection remains the modality of choice. However, endoscopic submucosal dissection (ESD) has been widely used for patients with early EAC. This report presents a patient with circumferential BE with multifocal EAC resected via ESD.
Case Description/Methods: Our patient is a 72-year-old male with a history of surgically treated lung cancer, prostate cancer in remission, and atrial fibrillation who presented with acute GI bleeding due to NSAID-induced peptic ulcer disease. Esophagogastroduodenoscopy (EGD) with biopsies showed BE (Prague C14M14) with high-grade dysplasia (HGD) and multifocal intramucosal EAC; however, no discrete mass was noted. PET scan showed mild increased metabolic activity in the distal esophagus. Endoscopic Ultrasound (EUS) showed no sonographic evidence of a mass or abnormal lymph nodes. After a multidisciplinary discussion, a circumferential ESD was performed with resection of the entire segment of BE en bloc (15 cm). Triamcinolone was injected to decrease the risk of stricture formation. Two overlapping covered stents were placed. Pathology revealed negative margins with three foci of invasive adenocarcinoma with submucosal invasion (< 500 microns) (pT1b). The patient was discharged the next day on high-dose PPI. Six weeks later, the stents were extracted successfully. One week later, the patient developed mild dysphagia. Repeat EGD showed short stricture that was dilated with a balloon. The patient remains asymptomatic, tolerating an oral diet with a plan for repeat EGD in two weeks for further dilation.
Discussion: Long Segment BE (LSBE) carries a higher malignant transformation risk than short segment. In a 6.4-year study of 1061 patients, LSBE progressed to EAC annually at 0.25%. ESD is preferred for early-stage EAC, offering en-bloc resection of large lesions and lower recurrence rates than EMR. The American Society of Gastroenterology Guidelines (ASGE) recommends ESD over EMR for early-stage EAC (T1) or Barret's nodular dysplasia >20mm. This further supports ESD use in our case. Long-segment ESD risks stricture formation and intraprocedural micro perforation. Only a few cases of ultra-long BE treated via ESD are documented; to our knowledge, our case is the longest.
Disclosures:
Aida Saad, MD1, Arshia Khorasanizadeh, MD2, Kais Zakharia, MD3, Joyce Arnouk, 4. P2851 - Circumferential Endoscopic Submucosal Dissection (ESD) of 15-cm Long Segment Barrett’s Esophagus With Multi-Focal Intramucosal Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Aida Saad, MD1, Arshia Khorasanizadeh, MD2, Kais Zakharia, MD3, Joyce Arnouk, 4
1Baystate Medical Center, Enfield, CT; 2UMass Chan, Baystate, Springfield, MA; 3Baystate Medical Center, Springfield, MA; 4Westfield, MA
Introduction: Barret's esophagus (BE) is a well-known precursor of adenocarcinoma. Endoscopic mucosal resection (EMR) and ablation therapy (radiofrequency ablation and cryotherapy) are the mainstay of treatment for dysplastic BE. For patients with locally advanced esophageal adenocarcinoma (EAC), surgical resection remains the modality of choice. However, endoscopic submucosal dissection (ESD) has been widely used for patients with early EAC. This report presents a patient with circumferential BE with multifocal EAC resected via ESD.
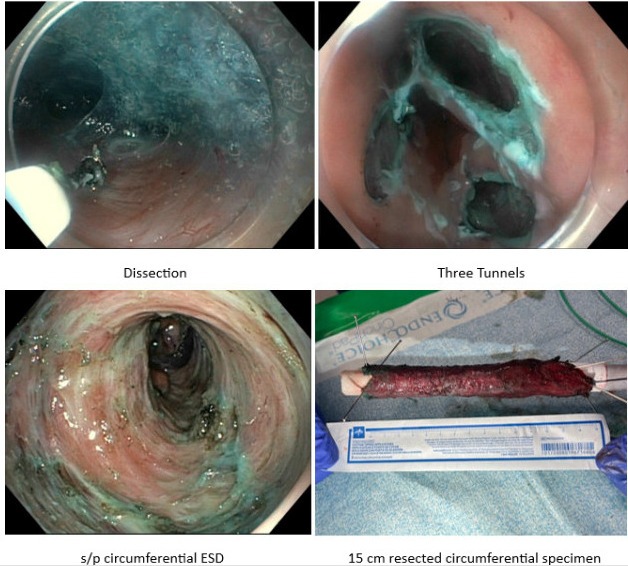
Case Description/Methods: Our patient is a 72-year-old male with a history of surgically treated lung cancer, prostate cancer in remission, and atrial fibrillation who presented with acute GI bleeding due to NSAID-induced peptic ulcer disease. Esophagogastroduodenoscopy (EGD) with biopsies showed BE (Prague C14M14) with high-grade dysplasia (HGD) and multifocal intramucosal EAC; however, no discrete mass was noted. PET scan showed mild increased metabolic activity in the distal esophagus. Endoscopic Ultrasound (EUS) showed no sonographic evidence of a mass or abnormal lymph nodes. After a multidisciplinary discussion, a circumferential ESD was performed with resection of the entire segment of BE en bloc (15 cm). Triamcinolone was injected to decrease the risk of stricture formation. Two overlapping covered stents were placed. Pathology revealed negative margins with three foci of invasive adenocarcinoma with submucosal invasion (< 500 microns) (pT1b). The patient was discharged the next day on high-dose PPI. Six weeks later, the stents were extracted successfully. One week later, the patient developed mild dysphagia. Repeat EGD showed short stricture that was dilated with a balloon. The patient remains asymptomatic, tolerating an oral diet with a plan for repeat EGD in two weeks for further dilation.
Discussion: Long Segment BE (LSBE) carries a higher malignant transformation risk than short segment. In a 6.4-year study of 1061 patients, LSBE progressed to EAC annually at 0.25%. ESD is preferred for early-stage EAC, offering en-bloc resection of large lesions and lower recurrence rates than EMR. The American Society of Gastroenterology Guidelines (ASGE) recommends ESD over EMR for early-stage EAC (T1) or Barret's nodular dysplasia >20mm. This further supports ESD use in our case. Long-segment ESD risks stricture formation and intraprocedural micro perforation. Only a few cases of ultra-long BE treated via ESD are documented; to our knowledge, our case is the longest.
Figure: Ultra-long segment ESD procedure steps.
Disclosures:
Aida Saad indicated no relevant financial relationships.
Arshia Khorasanizadeh indicated no relevant financial relationships.
Kais Zakharia indicated no relevant financial relationships.
Joyce Arnouk indicated no relevant financial relationships.
Aida Saad, MD1, Arshia Khorasanizadeh, MD2, Kais Zakharia, MD3, Joyce Arnouk, 4. P2851 - Circumferential Endoscopic Submucosal Dissection (ESD) of 15-cm Long Segment Barrett’s Esophagus With Multi-Focal Intramucosal Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

